Technology Can Be Used in Multiple Areas Including Healthcare, Climate Change, Managing Natural Disasters, Architecture, Urban Planning and Drug Design
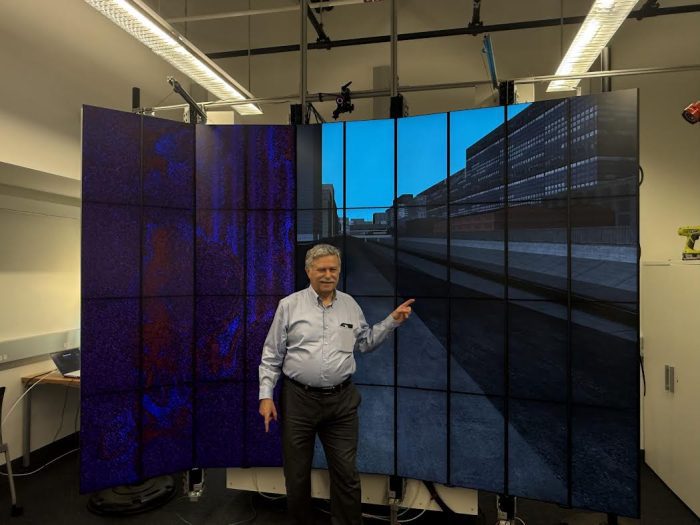
Stony Brook University’s Center for Visual Computing has completed construction of the FlexiCAVE—the world’s largest flexible, dynamically reconfigurable high-resolution stereo display facility. Housed on the first floor of the New Computer Science (NCS) building, the FlexiCAVE comprises 40 tiled, high-pixel-density monitors capable of rendering about 83 million pixels, all while physically transforming its shape to support a wide range of scientific and data-driven applications, improving immersive visualization technology.
“We envisioned a display that would adapt to the data—not the other way around,” said Arie Kaufman, distinguished professor of Computer Science and the principal investigator behind the project. “With FlexiCAVE, we’re enabling researchers to literally shape their workspace to the needs of their analysis.”
Innovative Interaction and Applications
Unlike traditional static visualization walls or even curved displays, the FlexiCAVE is built on a modular architecture with rotatable display columns. The system can seamlessly transition between flat, L-shaped, U-shaped, or semi-circular configurations in real time. These transitions are not only cosmetic. They directly influence the visualization, the user experience and the type of data interaction enabled.
A custom-built rendering engine powers the design that synchronizes stereo views and dynamically updates visualizations as users physically adjust the screen layout. The team calls this new interaction paradigm —PIVoT, which is an acronym for Physical Interaction to Virtual Transformation.
“It’s more than a screen. It’s a physical and tangible interface for virtual exploration where users are immersed in the data, and the layout of the FlexiCAVE anchors their sense of whereness, helping them stay oriented as they navigate complex visual spaces,” noted Principal Research Scientist Dr. Saeed Boorboor, co-author of the recently submitted VIS 2025 paper which details the system.
Real-World Applications
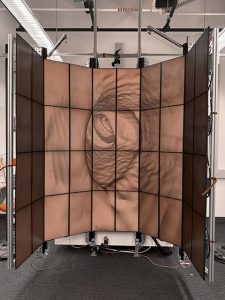
The team has already demonstrated real-world applications in many areas including healthcare. For example, virtual colonoscopy shifts the layout from a flat 2D overview of the patient’s colon to a curved immersive 3D endoluminal view (see Figure 2). In medical imaging visualization, radiologists can tangibly move the FlexiCAVE displays to virtually “slice” through brain MRI or abdominal CT scans.
And in situations like in urban flood simulations, emergency planners can orient and navigate flooding scenarios spatially by reconfiguring the display (see Figure 1).
In addition, researchers are using FlexiCAVE to experiment with multivariate data visualization, dynamically switching between scatter plots and parallel coordinate plots by physically bending screen segments. This hands-on interaction transforms the way users explore complex datasets. In an early user study, participants preferred the flexibility of the system and reported improved spatial perception over traditional static layouts. Other areas that can be enhanced include architecture, urban planning, geospatial data, biological systems, drug design, and many others.
Why Now?
As datasets continue to grow in both size and complexity—ranging from volumetric brain scans to climate models—there is a pressing need for immersive tools that allow researchers to explore data from multiple angles and scales. The FlexiCAVE, part of a growing trend in large high-resolution tiled displays,takes a bold step forward by combining stereoscopy, dynamic curvature, and tangible interaction into one unified system.
With backing from the New York State and Federal agencies, the FlexiCAVE’s development represents years of engineering insight, including customized aluminum framing, inclinometer-equipped hinges, and powerful GPU clusters capable of real-time image updates in a noise-canceling cabinet.
Looking Ahead
While the current version requires manual adjustment of the display columns—a design challenge acknowledged by the team—future updates may introduce motorized column rotation for ease of use. The research group is also exploring new applications in collaborative analytics and adaptable visualization workflows.
“We hope FlexiCAVE becomes a blueprint for the next generation of immersive environments—not only here at Stony Brook, but also globally,” said Professor Kaufman.