By Daniel Dunaief
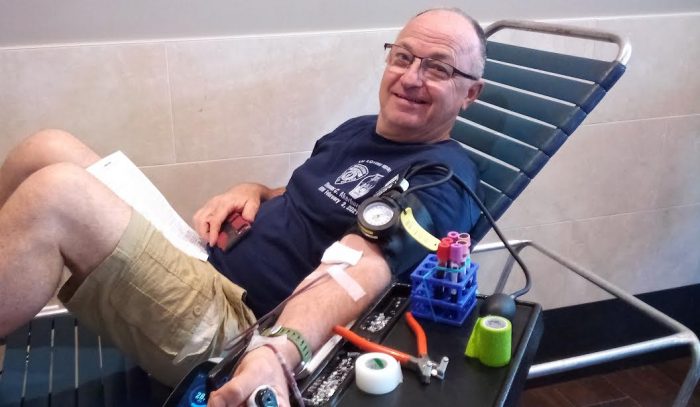
Ralph Sabatino, a lawyer and St. James resident, was in his bedroom, sitting at his computer when he fell out of his chair.

When his sister Maria, who was visiting from New Jersey in April of 2023, came into the room, she immediately called his wife Claire, a registered nurse, to come check on him.
“I noticed his left arm and left leg were paralyzed,” said Claire Sabatino, who has been married to Ralph for almost 44 years. “HIs speech was garbled.”
Claire called 911 and told the dispatcher that her husband was exhibiting the signs of a stroke. Within minutes, an EMS ambulance and one of the two Mobile Stroke Units from Stony Brook hospital arrived.
In the mobile stroke unit, technicians conducted a CAT scan, forwarding the results to Dr. David Fiorella, Director of the Stony Brook Cerebrovascular Center and Co-Director of the Stony Brook Cerebrovascular and Comprehensive Stroke Center at Stony Brook Medicine. When he arrived at the hospital, Sabatino bypassed the emergency room and went directly into an operating room.
Fearing the worst, Claire Sabatino called their adult daughter Gabrielle and told her to get to the hospital as quickly as possible.
“I never saw anybody with the symptoms my husband was exhibiting that fully recovered in the past,” she said. “When I saw him on the floor, I thought that would be the way he’d live for the rest of his life, if he survived. I wasn’t sure he would.”
After the stroke and the operation, Sabatino, who is now 68 years old, has no symptoms following what is far too often a life-altering condition.
“It’s sometimes hard for me to fathom how massive the stroke was because I have had no lingering effects,” he said.
Indeed, Sabatino estimates that the time between when he had the stroke until he was wheeled in the recovery room was about an hour and a half.
“Stroke is an emergency,” said Fiorella. “Although it’s not painful, numbness, weakness involving one side of the body, difficulty with speech, understanding speech, difficulty with vision, anything that presents acutely shouldn’t be ignored. It needs prompt attention.”
As a way to recognize the signs of stroke and the urgency to get help, doctors in this field suggest that people remember the acronym BE FAST, which stands for balance, eyes, face, arm, speech, time.
With seniors representing the fastest growing population on Long Island, residents and their families and caregivers need to be aware of stroke symptoms and, in the event of a stroke, to have an action plan in place.
“We have an aging population and the prevalence of stroke is increasing,” said Fiorella.
In Suffolk County, Stony Brook has two mobile stroke units, positioned on the Long Island Expressway at Exits 57 and 68. These units are located within 10 miles of 46 EMS territories.
Since Stony Brook started deploying these mobile stroke units in April of 2019, these specialized and life-saving ambulances have responded to about 8,000 stroke calls.
During those years, the hospital has demonstrated a significant reduction in time to treatment, with more patients receiving clot busting medications while in transit, and lower rates of mortality and morbidity, Fiorella explained.
A workup and diagnosis at other hospitals can take three or more hours, which a mobile stroke unit can perform with a CAT scan.
Additional benefits

Fiorella explained that the technicians in the ambulance share considerable information about the patient while in transit, including whatever contact numbers they could collect from family members on site.
Stony Brook Hospital can then begin a dialog with those family members, preparing them for any potential procedures and, if the patient is a candidate for a new treatment, receiving authorization.
A well-established and industry leading stroke unit, Stony Brook is involved in several experimental protocols designed to improve treatment.
“Whenever we can, we offer newer and better technologies,” said Fiorella. By participating, patients not only benefit from advances in the field, but also help the thousands who come after them. Patients can “make tremendous contributions to their own care and to medicine” amid developments and advanced technologies, he said.
In cases where patients or their representatives prefer not to use any advanced or newer technology, Stony Brook provides other life-saving services.
Fiorella added that the mobile stroke unit doesn’t only bring patients to Stony Brook, but also takes them to other comprehensive stroke centers for advanced treatment.
While strokes disproportionately affect the elderly, with the Medical University of South Carolina estimating that 75 percent of strokes occur in people 65 and older, certain conditions can increase the risk of strokes, such as smoking, vascular or heart disease, high blood pressure and peripheral vascular disease.
Another success story

Bill Rothmeier, who lives in Oakdale, was coming back from upstate in 2019 when his wife Eileen recognized that he was driving strangely.
She asked him to pull over so she could use the restroom. When she returned, she took over the driving. By the time they got home, Rothmeier’s ability to speak had declined.
Eileen Rothmeier spoke to a next door neighbor, who was involved with a community ambulance in Sayville. He had heard about the stroke unit.
“The next thing I knew, two ambulances were in front of my house,” said Bill Rothmeier, who is now 68. The MSU did a CAT scan and gave him a shot on the way to the hospital.
When he was in the recovery room, Rothmeier said Fiorella came in and told him he put in a stent and pulled two blood clots out of his brain.
“He said it like I was going out to a deli to get lunch,” said Rothmeier, who, as it turns out has owned the Lake Grove Deli for 29 years. “If it wasn’t for those guys,” including the MSU crew and Fiorella, “I could be in a nursing home or worse right now.”
Rothmeier was one of the first to receive life saving treatment through the mobile stroke unit and at the hospital.
A rewarding job
While the mobile stroke unit provides an important service for people battling a stroke, it doesn’t add any cost for the patient.
Stony Brook provides the units “free of charge,” because the “outcomes are so much better,” Fiorella said.
Patients who have untreated strokes or whose strokes are treated much later can have an irreversible brain injury, which could involve hospitalizations that last for months.
Stony Brook receives the same flat rate from Medicare for stroke victims, which helps provide financial support for the ambulance and is a “home run” for the patient, Fiorella added.
From Fiorella’s perspective, the opportunity to help people more than compensates for the 2 am calls he sometimes gets when he needs to come in for emergency surgery.
In the 25 years he’s been involved in stroke care, Fiorella has “never lost the fascination in how great the technology has become and how quickly it’s advanced,” he said. After treatment, people who couldn’t speak or understand speech and who couldn’t move the dominant side of their body can return to normal activities.
“It’s such a wonderful experience being involved with this,” he said. “I wouldn’t be able to do this without the support of Stony Brook.”
As for Claire Sabatino, who had never heard of the mobile stroke unit before the ambulance was parked on her driveway last April, the benefit of the rapid transit and the Stony Brook team is “nothing short of a miracle.