The Suffolk County Water Authority announced on June 10 that all treated water it supplies to customers is in full compliance with the federal drinking water standards for PFOA and PFOS—six years ahead of the 2031 compliance deadline set by the U.S. Environmental Protection Agency (EPA).
The EPA finalized a new enforceable standard of 4 parts per trillion (PPT) for both PFOA and PFOS in April 2024. SCWA’s testing this past April confirmed that no treated water in its system contained PFOA or PFOS above that level. This achievement comes despite the widespread presence of PFAS in Long Island’s aquifer.
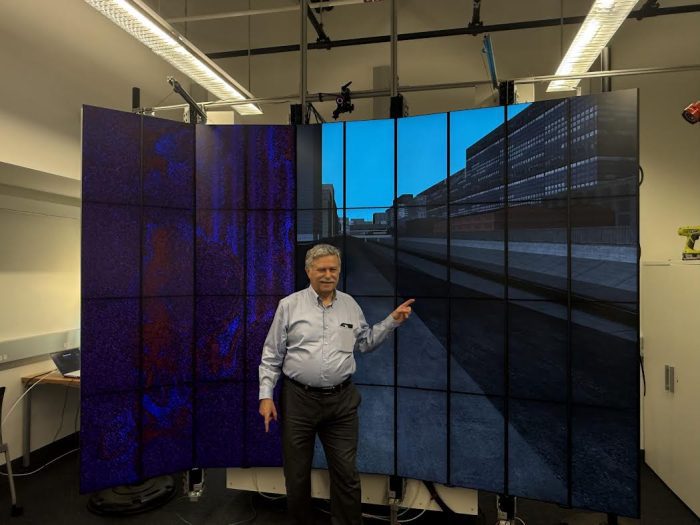
“Given the extent of PFAS detections across Long Island and the size of our system, this is a historic achievement,” said SCWA Chairman Charles Lefkowitz. “This result shows that with the right investment and urgency, we can stay ahead of emerging threats to public health.”
PFAS, or per- and polyfluoroalkyl substances, are a class of synthetic chemicals that have been widely used for decades in products such as non-stick cookware, stain-resistant fabrics, food packaging and firefighting foams. These substances do not break down easily and have leached into groundwater in many areas, including Long Island. Long-term exposure to certain PFAS compounds—particularly PFOA and PFOS—has been linked to health effects including developmental issues, hormone disruption and certain cancers.
To meet the new federal standards well ahead of schedule, SCWA installed 17 granular activated carbon (GAC) treatment systems for PFAS in the past year alone. GAC filters remove PFAS by adsorbing the contaminants onto specially prepared carbon. Water is passed through these large vessels, and the PFAS compounds adhere to the carbon, allowing clean water to continue through the system. Testing by SCWA shows that GAC removes PFAS compounds to non-detectable levels.
“This didn’t happen overnight,” said SCWA Chief Executive Officer Jeff Szabo. “We’ve been working for years to build a treatment program that protects our customers and anticipates regulatory changes. The fact that we’re already in compliance—years ahead of the federal deadline—speaks to the expertise of our team.”
SCWA continues to test regularly and will immediately remove any well from service if it detects PFOA or PFOS above 4 PPT if that well does not already have treatment in place. SCWA’s long-term goal is to supply water without any detectable levels of PFAS compounds, and additional treatment systems are planned for installation.
“This is about protecting public health,” said Suffolk County Executive Ed Romaine (R). “I want to thank the Suffolk County Water Authority for acting early and doing what’s necessary to provide residents with some of the cleanest drinking water in the country. Their leadership and investment in treatment technology are making a real difference.”
“Ensuring public safety and preserving our water quality are two of the highest priorities for me and my legislative colleagues. The leadership of the Suffolk County Water Authority has again shown its commitment to protecting the public, and in this case has exceeded expectations set by the federal government in achieving safer, even zero levels, of PFAS compounds in our water,” said Presiding Office Kevin J. McCaffrey.
“Clean drinking water is essential to public health, and PFAS contamination is a serious threat that demands action,” said Adrienne Esposito, Executive Director of Citizens Campaign for the Environment. “Meeting the federal standards well ahead of schedule is a positive step forward in safeguarding Suffolk’s residents.”
SCWA’s accelerated timeline has been supported in part by $16 million in grant funding awarded by New York State. These funds have helped offset the significant cost of installing advanced PFAS treatment systems, allowing SCWA to move faster while minimizing the financial impact on customers. By leveraging state support and working efficiently, SCWA has been able to continue delivering high-quality water at some of the lowest rates in New York.
“This is one of the largest groundwater systems in the country—and one of the most complex,” Lefkowitz added. “We’ve proven that even in a region with serious PFAS challenges, we can deliver water that meets the highest health standards.”
SCWA is an independent public-benefit corporation operating under the authority of the Public Authorities Law of the State of New York. Serving approximately 1.2 million Suffolk County residents, the Authority operates without taxing power on a not-for-profit basis.