By Daniel Dunaief

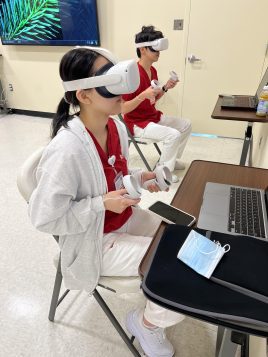
Photo from Stony Brook School of Nursing
People put their lives in the hands of unseen airline pilots who have enhanced and sharpened their skills using simulators. These simulators can prepare them for a wide range of conditions and unexpected challenges that enhance their confidence on the fly.
The same approach holds true for nurses, who seek to help patients whose symptoms may change even as the nurse is working with several people at the same time.
In an initiative designed to provide in depth training to nurses throughout the state, while filling a shortage of these vital professionals, New York State recently announced a $62 million contribution to three nursing simulation centers: SUNY Buffalo, SUNY Canton and Stony Brook University. With $10 million of state funds that the university will match with $10.5 million of its own money, SBU will increase the number of nurses it trains.
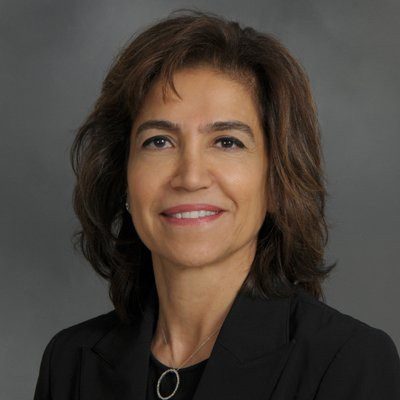
“We are very fortunate here at Stony Brook that we get many, many qualified applicants for our nursing program [for whom] we have not, to date, been able to offer seats,” said Dr. Patricia Bruckenthal, Dean of the School of Nursing at Stony Brook. This will enable the school, as well as the other programs, to train more students.
Effective training
While Stony Brook offers nursing simulation training, the additional funds will greatly expand the size and scope of that effort.
The NEXUS-Innovation Center, which stands for Nursing EXcellence Using Simulation, will take about two years to build and will have a phased in enrollment approach. In the third year, the school will add 56 baccalaureate nursing students. In the fifth year, Stony Brook will have space for 80 more students.
The current simulation center is about 1,850 square feet, which includes a nursing skills lab, exam room and debrief/ flex room.
The new center will add 15,000 square feet.
The simulation center will have 16 hospital style beds, with all the equipment nurses would normally see in a hospital room, including suction, air, oxygen, otoscope, ophthalmoscope, monitoring, and a call bell system. The center will also have eight examination rooms.
The proposal also includes the design of an apartment with a laundry, kitchen, bathroom and shower, helping train nurses who will help people in residential settings.
Among other features, the center will have a control room where instructors and operators manipulate the AV equipment and patient simulations, observe and document performance, collect data and prepare for debriefing.
Bruckenthal is planning to hire a faculty member in the next few months to become simulation coordinator who will work with the Director of the Learning Resource Center.
Within the next two years, Stony Brook anticipates hiring one more nursing faculty Clinical Simulation Educator and one Simulation Operations Specialist, who will ensure that all technical aspects of the center are functioning correctly. This new hire will also troubleshoot equipment, while performing emergency repairs on equipment and arranging for vendor repairs.
All of this equipment and expertise provides opportunities to create scenarios that build expertise. The conditions can change, as a patient goes from an expected outcome to one in which the conditions rapidly deteriorate.
In addition to expanding capacity and giving nurses an opportunity to understand and react to patients who have a wide range of conditions they might not see during routine clinical training, the center will also enable these students to build their competence and confidence in a low-stakes environment.
“It provides for a safe learning environment,” said Bruckenthal. “Students can make mistakes without risking patient safety. It’s much less stressful.”
Future nurses can also continue to work in the simulation lab on a particular skill until they feel confident in their abilities.
Several studies have validated the effectiveness of educating and preparing nurses in a simulated setting.
A landmark study in 2014 conducted by the National Council of State Boards of Nursing compared the clinical competence of nurses in training across three groups: one that had no simulation training, a group with 25 percent of their clinical training replaced by simulation, and a third group with 50 percent clinical training through simulation.
The nursing certification pass rate scores were the same for all three groups. Simulation trained nurses performed as well or better in areas like critical thinking and clinical judgment.
Additionally, follow up studies showed that employers found that nurses trained using high fidelity simulation were just as effective as those who were trained in the clinic in areas including patient safety, communication and evidence-based practices..
The center can also pivot to provide nurses with training for expanding local health threats, such as a simulated version of a measles outbreak, Lyme disease or a spike in other conditions that might cause a surge in hospital visits.
“We can build and design cases that meet those needs,” said Bruckenthal.
The center can build in disaster training, giving nurses a chance to interact with colleagues in other health professions during any of a host of other scenarios. When interacting with other healthcare professionals, nurses can practices the SBAR technique, in which they describe the Situation, provide Background, give an Assessment, and offer a Recommendation.
The expanded simulation center will incorporate design elements such as soundproofing, lighting and ventilation and will align with the university’s goals towards sustainability and green-oriented design.
Long term commitment
Bruckenthal has been contributing to Stony Brook for 44 years, ever since she graduated from the nursing school in 1981.
Her first job as a nurse was at the newly opened hospital. She and Carolyn Santora, Stony Brook Medicine Chief Nursing Officer, have worked together since 1981 and went through the Stony Brook master’s program together. They have established the Stony Brook Nursing Alliance.
Bruckenthal is energized by the opportunities ahead.
“Nursing is one of those careers where you can always keep yourself new and find new and exciting opportunities,” she said.
In the early days of her nursing career, she recalled that nurses weren’t exposed to all the types of conditions they might face in various settings.
“Having the opportunity to have nurses practice in this low risk environment and build that confidence and skills is a better way to prepare nurses to be ready for the work force,” she said
With nurses involved in so many aspects of patient care, Bruckenthal dreams of creating a nursing innovation incubator.
Nurses can offer insights into developing innovative ways to improve health care, whether working with biomedical engineers or biomedical informatics and can help design human-centered technology. Such a center could allow nurses to learn more about technology and business while enabling them to become leaders and entrepreneurs.
“Nurses have a problem-solving mindset,” Bruckenthal explained. “Sustainable and scalable solutions are really going to take a joint effort between educators, clinicians and industry partners.”