By Leah S. Dunaief

Publisher
Speaking of our health, which we often do with friends, there were a couple of interesting bits of news this week in that department.
Probably the most dramatic is the idea that by delaying the onset of menopause, a woman’s life and good health might be extended. The health benefits that women have before menopause lessen as we age past that mark. So current longevity research is asking if the whole picture could be slowed. And so, Dr. Jill Biden announced from the White House a new health initiative to pursue this concept, with Dr. Renee Wegrzyn steering the research.
Ovaries, which seem to play a role throughout a woman’s lifetime, not just until menopause, are the main focus. “Researchers think that prolonging their function, better aligning the length of their viability with that of other organs, could potentially alter the course of a woman’s health—and longevity research overall,” according to Tuesday’s front page story in The New York Times.
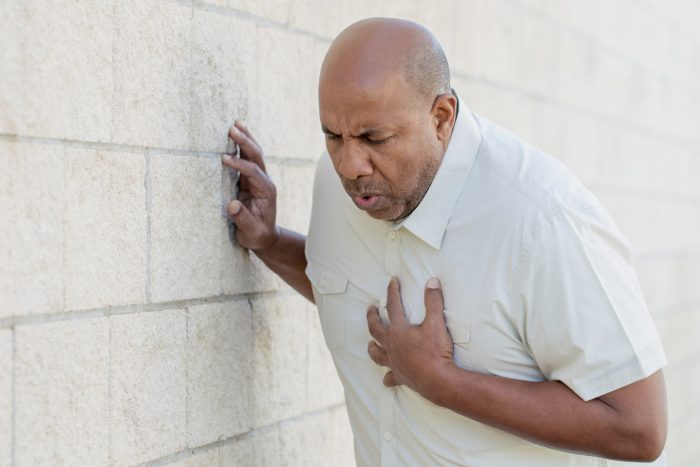
Using hormones like estrogen and progesterone, ovaries communicate with every other organ in the body. When they stop communicating, “all kinds of problems arise.” They stop when the eggs that they carry are gone, at which point risk increases for dementia, cardiovascular disease, osteoporosis and other age-related diseases and lifespan, according to The Times. Women whose ovaries have been prematurely removed for other health reasons are at greater risk, which suggests that even after all the eggs are gone, ovaries may still play a protective role.
All of this is subject to much further investigation. Researchers are not sure whether aging negatively affects the ovaries or if the ovaries cause other organs to age. But prolonging ovarian function in lab animals does seem to improve their health and longevity. This encourages further research into reducing the number of eggs lost by a woman during each menstrual cycle, thus preserving ovarian function. (Women shed may eggs many cycle but one ovulates). A current drug, rapamycin, which is an immunosuppressant used in organ transplants, is being studied for that role.
Anti-aging research is highly popular among scientists these days.
Another surprising article in the same issue of The Times, this one in the ScienceTimes section, has to do with our sense of smell. Though it lessens with age (and might as the result of infections, like Covid), “A diminished ability to smell is associated with worsening memory, cognition and overall well-being—as well as dementia and depression.” The good news is that such a situation may be reversible.
We can train our noses with smelling exercises, and our ability to smell, in turn, may improve not only depression but also help remember words faster. One explanation for this is “the areas of the brain involved in smelling are uniquely connected to parts involved in cognition, such as the prefrontal cortex.” Further to the point, “The olfactory system is the only sensory system that has a direct superhighway projection into the memory centers and the emotional centers of your brain,” according to Professor Michael Leon of the University of California, Irvine.
So take out products from your kitchen cabinets and alternately smell cinnamon, honey, coffee, wine or others and sniff each of them at least 30 seconds at a time, once in the morning and once more at night. Small studies have indicated this not only tests one’s power to smell but also enhance cognitive abilities.
Finally for this column, I would like to quote the Times’ article on the Walking Cure for Lower Back Pain. Although those with pain may be loathe to exercise, movement can strengthen muscles that support the back and ease the pain. This is a conclusion that is supported with any number of studies over the past few years.
“Researchers found that regular exercise combined with physical education was the most effective way to prevent lower back pain from recurring,” according to The NYT.
Walking can help strengthen the support muscles at the base of the spine. When they weaken, it can lead to pain.
So, as the song goes, “Shake, Shake, Shake Your Booty,” for good health.