By Daniel Dunaief
What are you planning to do this Saturday?
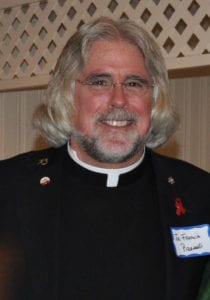
John Perkins, Community Outreach Manager at St. Charles Hospital and St. Catherine of Siena Hospital and Islip Terrace resident, is planning to swim 12.5 miles around Key West. The swim isn’t just an exercise in rugged outdoor activities or a test of his endurance, but is a way to raise money to support St. Charles Hospital’s stroke support group and promote stroke awareness and prevention.
As of Tuesday morning Perkins, who is 56 years old, has raised $4,900 out of his goal of collecting $5,000.
“Stroke survivors can have challenges for the rest of their lives,” said Perkins. “My hundreds of hours of training and hundreds of miles I’ve swam over the last year is nothing in comparison to someone who has a stroke” and then has a gate impairment, a speech impediment or is visually impaired.
Perkins added that about 80 percent of the estimated 800,000 strokes in the United States are preventable, through efforts like managing high blood pressure and/or diabetes, increasing physical activity and eating a healthier diet.
Perkins hopes the money he raises can add a new piece of equipment in the emergency room or help with the stroke survivor and support group.
Challenging conditions, with help
Getting ready for this swim took considerable work, especially given that Perkins didn’t even know how to swim until he was 50.
That’s when a group of childhood friends called him up in 2017 and suggested he join them for a two mile swim in the Straight of Messina, between Sicily and Calabria.
He rose to the challenge and raised $1,200.
To prepare for this much longer swim, which he estimates could take eight hours of more, he has been getting up at 4 am and is in the pool by 5 a.m.
Three days during the week, he swims two miles before work, often surrounded by people who are training for grueling races like triathlons and ironman competitions. On weekends, he does longer swims. He has been increasing the distances he swims in the pool, recently covering 10 miles in six and a half hours.
When he’s doing these longer swims, he gets out of the pool every two miles to take a 30-second break, which could involve hydrating and a quick restroom stop.
“You can not be a marathon swimmer without considering the nutrition aspect,” he said.
When he’s swimming around Key West, he plans to bring a special blend of carbohydrates, with calcium and magnesium and some protein, making sure he consumes about 300 calories per hour.
In expending over 6,000 calories for the swim itself, he wants to ensure he doesn’t tire or get cramps.
When he swims around Key West, Perkins said his wife Pamela, who is a registered nurse and whom he calls his chief nutritionist, will be in a two-person kayak. She will signal to him every 20 minutes or so to take a break for some liquid nutrition.
Meanwhile, his chief navigation officer, Michael Gugliotti, whom he also refers to as his “water Sherpa,” will ensure that he stays the course, not straying from the checkpoints so that he doesn’t wind up adding any distance to the long swim.
When he’s swimming, Perkins tends to think about the struggles stroke survivors have that they have to deal with for the rest of their lives.
“Strokes impact your life, your community’s life, your family’s life,” he said.
People interested in donating can do so through the following link: St. Charles Host Your Own Fundraiser