By Daniel Dunaief
Symptoms can range from dizziness and lightheadedness on standing to an inability to get out of bed.
These symptoms, which are characteristic of several medical conditions, are at the heart of a condition called Postural Orthostatic Tachycardia Syndrome, or POTS.
Affecting considerably more women than men, POTS, which is caused by a sudden and sometimes dramatic increase in heart rate when people stand, can be anything from a nuisance to a debilitating condition.
On Saturday, April 26, at 9 a.m. to 4 p.m., several doctors, working with Dysautnomia International, will present information at a continuing medical education course at the MART auditorium at Stony Brook University about POTS, which people can also attend virtually. Details and registration can be found below. This course is designed for medical professionals, but patients and caregivers are welcome to register too.
The condition is triggered by a problem with the autonomic nervous system, which controls heart rate, blood pressure, digestion and temperature regulation among other functions.
“I’ve had patients who were previously athletes who can’t exercise anymore,” said Dr. Jeffrey Boris, a pediatric cardiologist with a private practice, an expert in POTS, and one of the speakers at the course at Stony Brook.
In a previous study Boris conducted, he found that two out of three of his POTS patients had at least 10 symptoms, while half of them had at least 14 symptoms and 30 percent had at least 26 symptoms.
“The degree of debility can vary from some exercise intolerance to pretty much unable to get out of bed,” said Boris, who sees patients exclusively through telehealth and who is licensed to practice medicine in 18 states, not including New York.
An estimated one to three million Americans had some form of POTS before Covid. That number has increased to as many as six million.
Often triggered by an infection like the Epstein Barr virus, which causes mononucleosis, by Lyme Disease or even by concussions, POTS has no specific standard of care, as doctors have used a variety of pharmacological and non pharmacological treatments to help people suffering with these symptoms.
Some studies suggest that genetics plays a role in contributing to the disease.
Several high profile women have shared their battles with POTS, including Olympic gold-medal swimmer Katie Ledecky and Tori Moore, the wife of Super Bowl winning quarterback Nick Foles. Some doctors recommend swimming to POTS patients.
Medical education
The health care field hasn’t focused as much on POTS as it does on other diseases or conditions.
Doctors don’t always recognize POTS because they never learned about it in school, don’t believe it exists or didn’t train for this in their specialty work, Boris said.
The combination of these factors makes it harder for patients to receive a diagnosis.
Additionally, several other conditions have similar symptoms, including thyroid disease, low vitamin D, low iron and Addison’s Disease, among others.
The average patient takes four years to get an accurate diagnosis, according to Lauren Stiles, founder and president of Dysautonomia International (DI) and Research Assistant Professor of Neurology at the Renaissance School of Medicine at Stony Brook University. Stiles is the course co-chair for the POTS.
Indeed, Jennifer Samghabadi, who works as a registered nurse for neurologist Dr. Mark Gudesblatt, had symptoms of POTS as early as 2004, but didn’t receive a diagnosis until after her symptoms worsened in 2012 following a bout with swine flu.
POTS “is often misdiagnosed,” said Samghabadi, who is a resident of Port Jefferson Station. “Symptoms mimic so many other things. Your autonomic nervous system is misfiring in every which way.”
Stiles, who founded DI in 2012 and has created support groups in over 80 countries for people who suffer from this condition, has been working with medical schools around the country to create more training for doctors.
Patients are typically treated through a combination of pharmacological and non pharmacological approaches. The medicines they have used, including ivabradine, have been approved for the treatment of other conditions and are used in an off-label basis.
Boris is planning to talk to doctors about various types of treatments he’s used that work.
“I can’t routinely predict what therapies are going to help,” Boris said. “It’s really variable from patient to patient. It can be a lot of trial and error.”
Non-pharmacological treatments include elevating the head of the bed frame about six to eight inches. That can cause the kidneys to hold onto salt and water, which can lesson symptoms, Boris explained.
Additionally, doctors recommend a high salt, high liquid diet, which can include three liters or more of water each day.
Boris has had some success working with abdominal binders, which he has found are more effective than compression stockings.
To be sure, some patients have gastrointestinal issues, including nausea, bloating and constipation. For those patients, as well as people who have autism spectrum disorder, abdominal pressure won’t likely provide any relief and may make some symptoms or discomfort worse.
In the talk Boris is giving, he would like doctors to recognize that the disease exists, it’s validated and it’s something that, if health care professionals are creative and thoughtful, they can find possible treatment options for patients who are often suffering through different levels of symptoms.
At this point, federal funding for research into POTS stands at about $4 million per year, which is up from $2 million per year before Covid, but is still short of what doctors and advocates would like to see for a potentially debilitating disease.
Boris hopes that further research will provide a better idea of what is leading to POTS, which may lead to a Food and Drug Administration-approved treatment.
People who wants to learn more about the condition can visit the web site CurePOTS.org. Dysautonomia International offers a list of doctors skilled in diagnosing and treating POTS as well as other autonomic disorders.
Samghabadi, who is on the board of DI, urged medical care professionals to attend the course.
“It’s going to teach you everything you need,” she said. “It’s practical, evidence-based strategies for diagnosing and treating dysautonomia and is immediately applicable to patients.”
Even doctors who don’t think they can treat these patients should be aware of it so they know where to send patients, she suggested.
——————————————————————-
DETAILS AND REGISTRATION:
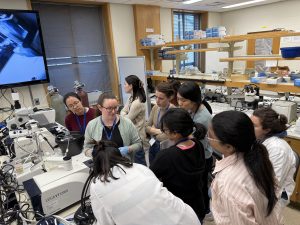
Dysautonomia International and Stony Brook University School of Medicine invite you to join us for a Continuing Medical Education course, Updates in Postural Orthostatic Tachycardia Syndrome Clinical Care & Research, on Saturday, April 26, 2025, 9am-4pm ET, held at the Stony Brook University MART Auditorium.
A networking reception with light refreshments will be held from 4 to 5 p.m. after the course.
Advanced registration is required. Up to 5.50 AMA PRA Category 1 Credit(s)™ are available for online or in person CME registrants. Please see the event website for details on CME credits. The lectures will be recorded and made available to all registered guests after the live event. CME credit is only available by watching the live broadcast or attending in person.
In Person Registration Fees:
Stony Brook University Students, Faculty & Staff (with CME credit): FREE
Community Physicians (with CME credit): $100
RN, PT, OT, Allied Health: (with CME credit): $75
Patients & Caregivers/Public (no CME credit): $25
Livestream Registration Fees:
Stony Brook University Students, Faculty & Staff (with CME credit): FREE
Livestream with CME credit: $100
Livestream with no CME credit: $25
If you are unable to attend in person or watch the livestream, but would like access to the recorded lectures, you can register for the “Livestream with no CME credit” option.
Online and in person registration options are available at bit.ly/StonyBrookCME