Health professionals from St. Catherine of Siena Hospital will be available at Sunken Meadow State Park’s boardwalk in Kings Park on Tuesdays, May 14, 21 and 28 from 5 to 7 p.m. to discuss heart health, healthy eating, weight management, breast health, stroke prevention, skin cancer and Lyme disease prevention tips. Free blood pressure screenings and free giveaways. To learn more, call 631-870-3444.
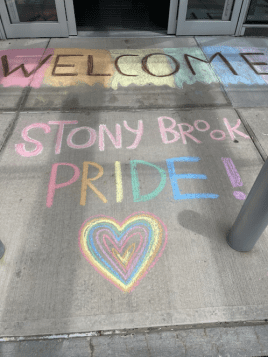
All Stony Brook Medicine hospitals named national leaders in LGBTQ+ healthcare equality
Stony Brook University Hospital (SBUH), Stony Brook Children’s Hospital, Stony Brook Southampton Hospital (SBSH) and Stony Brook Eastern Long Island Hospital (SBELIH) have been named “LGBTQ+ Healthcare Equality Leaders” for 2024 in the Human Rights Campaign Foundation’s Healthcare Equality Index (HEI). All hospitals received the top score of 100 on a survey encompassing non-discrimination and staff training, patient services and support, employee benefits and policies, and patient and community engagement.
“We are honored to be recognized as LGBTQ+ Healthcare Equality Leaders by the Human Rights Campaign Foundation’s Healthcare Equality Index,” said William A. Wertheim, MD, MBA, Interim Executive Vice President for Stony Brook Medicine. “This recognition reaffirms our unwavering commitment to providing inclusive and equitable care to all individuals, regardless of sexual orientation, gender identity or expression. We stand as advocates for diversity, champions for equality and partners in health for every member of our community.”
Stony Brook Medicine continues to grow its dynamic LGBTQ+ Committee, amongst all of its hospitals, to address the needs of the LGBTQ+ community, including patients, faculty, staff and trainees. The Stony Brook Medicine LGBTQ+ Committee is co-chaired by three SBUH-affiliated colleagues: Rose Cardin, MSN, RN, Director, Patient Education, Stony Brook University Hospital; Allison Eliscu, MD, FAAP, Chief, Adolescent Medicine, Stony Brook Children’s Hospital; and Adam Gonzalez, PhD, Vice Chair, Behavioral Health, Stony Brook Medicine. The multidisciplinary group is made up of medical and behavioral health providers and trainees, nurses, students, education specialists, and representatives from Human Resources, Information Technology and hospital administration. Its mission is to review, address and affirm the specific and unique needs of LGBTQ+ individuals, as well as promote respectful and culturally sensitive care to the LGBTQ+ community.
Each year SBUH seeks new ways to address and affirm the specific and unique needs of LGBTQ+ individuals. In 2023, SBUH updated their electronic medical record to add pronouns to the banner bar, so they are front and center for healthcare workers. Pronouns are words used to refer to either the person who is talking (like “I” or “you”) or a person being talked about in the third person (like “she/her,” “he/him,” and “they/them”). “They/Them” are common gender neutral pronouns. Being intentional about using someone’s pronouns is a simple way to show respect. Another accomplishment in 2023, SBUH scholars published results from Stony Brook Medicine’s LGBTQ+ Health Needs Assessment Survey, a collaborative effort in 2021 involving over 30 Long Island-based organizations and community leaders. Survey results are being utilized to guide our health system’s efforts to address health equity for the LGBTQ+ community.
A core mission for SBUH is fostering health equity for both its patients and staff. This past February, Stony Brook University Hospital was among the first eight hospitals in the United States to attain the Health Care Equity Certification from The Joint Commission and the only awarded organization on Long Island. Recognition was given to SBUH for implementing exemplary practices, such as employing health equity screening and data collection tools, documenting social work effectively, and making accommodations to meet the needs of patients with disabilities, among other activities.
“This recognition is a testament to the meaningful work carried out at Stony Brook University Hospital each day in support of the LGBTQ+ community on Long Island,” said Carol A. Gomes, chief executive officer for Stony Brook University Hospital. “For decades, our healthcare system has developed programs and offered services to help patients access the highest quality of care, and we want to continue to build on that strong foundation.”
Stony Brook Southampton Hospital’s Rose Walton Care Services has administered HIV prevention and care since the 1990s. In 2021, the hospital expanded services to include LGBTQ+ healthcare and opened the Edie Windsor Healthcare Center in Hampton Bays. The practice has a dedicated, full-time physician, Dr. Eric Lella, and provides confidential medical services in an accessible and caring environment, affirming all sexual orientations and gender identities and expression.
In 2023, SBSH implemented a LGBTQ+ Health Equity and Education Initiative program focusing on further educating staff in LGBTQ+ health care services, needs and protocols, including pronoun identification. The Edie Windsor Healthcare Center (through a NYSDOH AIDS Institute subcontract with PFY™) expanded mental health services and case management services, and the Center introduced patient navigation services to assist with insurance enrollment and access to entitlements/benefits, medical and other supportive services. The Center continues to administer mpox vaccinations to those who have been exposed to mpox or are at risk.
“The HEI Leadership designation recognizes our unyielding commitment to educate our staff in providing high-level LGBTQ+ healthcare with respect,” said Fredric I. Weinbaum, MD, CMO, COO and Interim CAO, Stony Brook Southampton Hospital. “As well as our efforts to provide LGBTQ+ patients with access to resources, programs and services.”
Stony Brook Southampton’s Hospital’s Diversity, Equity, and Inclusion Leadership Council, a committee of 25 administrators, physicians, nurses, and other staff, actively educates, informs, and provides resources for the wider hospital community about diversity issues while seeking opportunities to build an inclusive and safe environment for all who work in, seek care at, or visit the hospital’s facilities. To foster a sense of inclusion and compassion for all, the hospital has provided training to staff through the Responding to Equity, Diversity and Inclusion (REDI) program and the Greater New York Hospital Association’s Cultural Competency and Health Literacy education programs.
Upon reviewing HEI recommendations and criteria to better understand the behavioral health and medical needs of its local LGBTQ+ community, SBELIH revised human resource and hospital-wide policies, employee documents, terminology in medical records and facility signage. The changes enhanced SBELIH’s already strong focus on providing non-discriminatory and compassionate care. With a long history of serving the LGBTQ+ community, SBELIH continues to add clinicians and other staff members who specialize in LGBTQ+ care. The hospital’s history of service contributed to HEI naming SBELIH a Leader in LGBTQ Healthcare Equality.
SBELIH proudly participated in several initiatives promoting LGBTQ health equality. In June 2023, we joined the Greenport Pride Parade, demonstrating Stony Brook’s commitment to inclusivity and diversity. Collaborating with SBSH Edie Windsor Healthcare Center, SBELIH presented “LGTBQ* and Healthcare: Empowering Health, Embracing Diversity, in Southold NY,” underscoring the importance of LGBTQ-inclusive healthcare practices.
Additionally, SBELIH took part in “Queer Pride & Progress” by QUEERLI, in Jamesport NY, an event emphasizing inclusivity and understanding. Discussions covered a range of topics, including gender and sexuality, pronoun usage, and fostering a culture of care. SBELIH’s Chief Nursing Officer Suzie Marriott provided impactful contributions to these conversations.
“Ensuring health equity for all, regardless of sexual orientation or gender identity, is not just a moral imperative but a fundamental aspect of our commitment to compassionate care and inclusivity,” said Paul Connor, Chief Administrative Officer of Stony Brook Eastern Long Island Hospital. “Let’s continue to educate ourselves, engage in positive dialogue, and respect each other’s identities. Together, we can cultivate a world where everyone feels accepted and valued.”
The Human Rights Campaign Foundation is the educational arm of America’s largest civil rights organization working to achieve equality for lesbian, gay, bisexual, transgender and queer people. HRC envisions a world where LGBTQ+ people are embraced as full members of society at home, at work and in every community.
Stony Brook Medicine offers a range of specialized LGBTQ+ health services including a Talking About Gender (TAG) support group for teens to explore gender identity and expression, and a free educational support group for Parents of Transgender and Gender Diverse Children. For more information on Stony Brook Medicine’s LGBTQ+ care, visit:stonybrookmedicine.edu/LGBTQ.
Medical Compass: It’s not really about the salt shaker
Sodium’s effects are insidious
By David Dunaief, M.D.

Most of us consume far too much sodium. Americans consume an average of 3400 mg per day, well over the recommended 2300 mg per day recommended upper limit for those who are 14 and over (1). These consumption numbers are even higher for some demographics. It’s become such a health problem that the FDA is getting involved, working with food manufacturers and restaurants to drive these numbers down (2).
Why all the concern? Because even if we don’t have hypertension, sodium can have a dramatic impact on our health.
Sodium is everywhere, including in foods that don’t taste salty. Bread products are among the worst offenders. Other foods with substantial amounts of sodium include cold cuts and cured meats, cheeses, pizza, poultry, soups, pastas, sauces and, of course, snack foods. Packaged foods and those prepared by restaurants are where most of our consumption occurs.
On the flip side, only about two percent of people get enough potassium from their diets (3). According to the National Institutes of Health, adequate intake of potassium is between 2600 mg and 3400 mg for adult women and men, respectively.
What is the relationship between sodium and potassium?
A high sodium-to-potassium ratio increases our risk of cardiovascular disease by 46 percent, according to a 15-year study of more than 12,000 (4). To improve our overall health, we need to shift the sodium-to-potassium balance so that we consume more potassium and less sodium. And if you struggle with – or are at risk for – high blood pressure, this approach could help you win the battle.
Why lower your sodium consumption?
Two studies illustrate the benefits of reducing sodium in high blood pressure and normotensive (normal blood pressure) patients, ultimately preventing cardiovascular disease, including heart disease and stroke.
The first was a meta-analysis that evaluated data from 34 randomized clinical trials, totaling more than 3,200 participants. It demonstrated that salt reduction from 9-to-12 grams per day to 5-to-6 grams per day had a dramatic effect. Blood pressure was reduced by a significant mean of −4.18 mm Hg systolic (top number) and −2.06 mm Hg diastolic (bottom number) involving both normotensive and hypertensive participants (5).
When looking solely at hypertensive patients, the reduction was even greater, with a systolic blood pressure reduction of −5.39 mm Hg and a diastolic reduction of −2.82 mm Hg. The researchers believe that the more we reduce the salt intake, the greater the effect of reducing blood pressure. The authors recommend further reduction to 3 grams per day as a long-term target for the population and concluded that the effects on blood pressure will most likely result in a decrease in cardiovascular disease.
In the second study, a meta-analysis of 42 clinical trials including both adults and children, there was a similarly significant reduction in both systolic and diastolic blood pressures (6). Both demographics saw a blood pressure reduction, although the effect was greater in adults. Interestingly, an increase in sodium caused a 24 percent increased risk of stroke incidence but, more importantly, a 63 percent increased risk of stroke mortality. The risk of mortality from heart disease was increased alongside an increase in sodium, as well, by 32 percent.
Can you consume too little sodium?
Some experts warn that too-low sodium levels can be a problem. While this is true, it’s very rare, unless you take medication or have a health condition that depletes sodium. We hide sodium everywhere, so even if you don’t use a salt shaker, you’re probably consuming more than the recommended amount of sodium.
Why is potassium consumption important?
In a meta-analysis involving 32 studies, results showed that as the amount of potassium was increased, systolic blood pressure decreased significantly (7). When foods containing 3.5 to 4.7 grams of potassium were consumed, there was an impressive −7.16 mm Hg reduction in systolic blood pressure with high blood pressure patients. Anything more than this amount of potassium did not provide additional benefit. Increased potassium intake also reduced the risk of stroke by 24 percent.
Blood pressure reduction was greater with increased potassium consumption than with sodium restriction, although this was not a head-to-head comparison. The good news is that it’s easy to increase your potassium intake; it’s found in many whole foods and is richest in fruits, vegetables, beans and legumes.
The bottom line: decrease your sodium intake and increase potassium intake from foods. First, consume less sodium, and give yourself a brief period to adapt — it takes about six weeks to retrain your taste buds. You can also improve your odds by increasing your dietary potassium intake, striking a better sodium-to-potassium balance.
References:
(1) Dietary Reference Intakes for Sodium and Potassium. Washington (DC): National Academies Press (US); 2019 Mar. (2) fda.gov. (3) nih.gov. (4) Arch Intern Med. 2011;171(13):1183-1191. (5) BMJ. 2013 Apr 3;346:f1325. (6) BMJ. 2013 Apr 3;346:f1326. (7) BMJ. 2013; 346:f1378.
Dr. David Dunaief is a speaker, author and local lifestyle medicine physician focusing on the integration of medicine, nutrition, fitness and stress management. For further information, visit www.medicalcompassmd.com or consult your personal physician.
Walk with Mather Hospital for the fight against breast cancer on May 19
Join Mather Hospital, 75 North Country Road, Port Jefferson for the annual Northwell Health Walk at Port Jefferson to support the Fortunato Breast Health Center on Sunday, May 19
Presented by Bethpage Federal Credit Union, the Walk brings together family, friends and team members for a five-mile walk through the scenic villages of Port Jefferson and Belle Terre. The day includes music, raffles, photo props, a walker warm up session, and our popular Pink Your Pooch contest for the best “pinked” pup!
Sponsored by New York Cancer & Blood Specialists and CSDNET, the Northwell Health Walk at Port Jefferson benefits the Fortunato Breast Health Center and serves to raise awareness of the need for regular breast cancer screenings starting at age 40. Breast cancer is the most common cancer in women in the United States, except for skin cancers. It accounts for about 30% (or 1 in 3) of all new female cancers each year. The American Cancer Society estimates that in 2024 about 310,720 new cases of invasive breast cancer will be diagnosed in women and about 42,250 women will die from breast cancer.
Walk for a family member or friend fighting breast cancer, a breast cancer survivor, or in memory of someone whose life was cut short by this disease. Helpto raise funds for the Walk and collect Walk Fundraising Rewards! Participants can begin earning rewards by raising just $100! All rewards will be waiting for you at the Walk. Form a team with family, friends, or co-workers, join a team or walk as an individual, or sponsor a team or walker. Sign up for the Northwell Health Walk at Port Jefferson at Port Jefferson and we’ll see you on May 19!
Registration opens at 8 a.m and the Walk steps-off at 10 a.m. For more information or to register in advance, visit www.northwellhealthwalk.com.
Dr. Sanjay Galhotra joins Stony Brook Medicine physician network
Sanjay Galhotra, MD, FACP, DABOM, and the newly established Suffolk Primary Care, 200 Motor Parkway, Suite C-16, Hauppauge have joined Stony Brook Medicine Community Medical Group, Stony Brook Medicine’s expanding network of community practices.
“We are excited to have Dr. Sanjay Galhotra and his practice join,” said Dara Brener, MD, Clinical Quality Director of Stony Brook Medicine Community Medical Group. “His experience and dedication to his patients’ health and well-being will be a great asset.”
Dr. Galhotra is board-certified in internal medicine and obesity medicine and has more than 10 years of experience working as a hospitalist.
“I am very excited to join Stony Brook Medicine Community Medical Group,” said Dr. Galhotra. “I look forward to collaborating with other providers to provide excellent medical care to our patients. To make an appointment, call 934-213-4830.
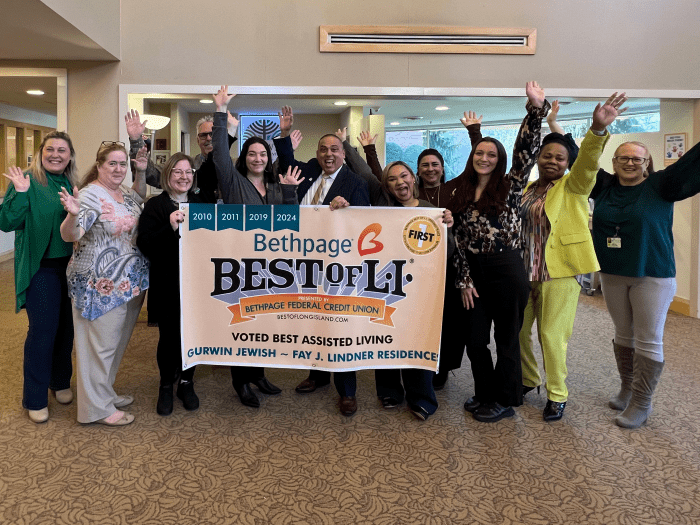
Gurwin Healthcare System sweeps 2024 Best of Long Island health & wellness awards
Gurwin Healthcare System has announced that it has received the following awards across various categories in the health and wellness category industry Bethpage Federal Credit Union’s 2024 Best of Long Island Awards:
- Julie Yerkes, RN voted Best Nurse for the second consecutive year.
- Gurwin Adult Day Health Program voted Best Adult Day Care Program for the eighth consecutive year.
- Gurwin Jewish Nursing & Rehabilitation Center voted Best Rehabilitation for the fourth consecutive year.
- Gurwin Home Care Agency voted Best Health Aides for the sixth consecutive year.
- Gurwin Jewish Nursing & Rehabilitation Center voted Best Nursing Home. The Center also received this honor in 2021.
- Gurwin Jewish ~ Fay J. Lindner Residences voted Best Assisted Living. The assisted living community also received this honor in 2010, 2011 and 2019.
The annual Bethpage Best of Long Island contest is a roadmap to the best businesses and services throughout both Nassau and Suffolk counties. This year, more than one million votes were cast by Long Island residents and patrons, who each voted in dozens of categories.
“We are delighted that Long Islanders have chosen so many of Gurwin’s programs as the Best on Long Island,” said Stuart B. Almer, President and CEO of Gurwin Healthcare System. “This recognition stems from the talented staff on the Gurwin team whose dedication is evident in their compassionate care and innovative programming. We are privileged to serve as a steadfast resource for thousands of older and medically frail adults in our surrounding communities and are honored to be recognized for our commitment to 5-star quality, patient-centered care.”
To view the complete list of winners, visit https://www.bestoflongisland.com/
About Gurwin Healthcare System
Gurwin Healthcare System is a renowned healthcare provider offering a full continuum of healthcare and senior living services for more than 35 years. Set on a 36-acre campus in Commack, NY, the System includes Gurwin Jewish Nursing & Rehabilitation Center, providing short-term rehabilitation and long-term skilled nursing care, memory care, respiratory and ventilator care, palliative and hospice care, social and medical adult day programs and on-site dialysis. Located within the Center is Gurwin Licensed Home Care Services Agency and Certified Home Care Agency, which provide in-home skilled care as well as home health aides. Sharing the campus is Gurwin’s Assisted Living community, Gurwin Jewish ~ Fay J. Lindner Residences, and Fountaingate Gardens, a luxury independent living community. Completing the Gurwin family of healthcare services is Island Nursing and Rehab Center, a 120-bed skilled nursing facility located in Holtsville, New York. For more information, visit www.gurwin.org. Follow Gurwin on Facebook (@GurwinNursingRehab) (@GurwinAssistedLiving) and on X (@GurwinJewish).
Jefferson’s Ferry Foundation welcomes supporters and residents to enjoy a ‘A New York State of Mind’ at its 19th annual Gala

Popular Fundraiser Benefits the Foundation’s Resident Assistance Fund
Every spring for nearly 20 years, Jefferson’s Ferry residents, donors, and vendors have joined Jefferson’s Ferry management, staff and board members to support the Jefferson’s Ferry Foundation at its annual gala fundraiser on April 18. This year was no exception. The party, held at Flowerfield in St. James, celebrated the vibrant community, active lifestyle, and peace of mind that can be found in abundance at Jefferson’s Ferry.
All proceeds from the evening will benefit the Foundation’s Resident Assistance Fund, which was established in 2006 to provide financial assistance to Jefferson’s Ferry residents who outlive their assets or experience a shortfall through no fault of their own. Over the years, the Resident Assistance Fund has played a role in upholding the Life Plan Community Promise of peace of mind and health care for Jefferson’s Ferry residents by subsidizing the monthly fees of residents in need.
This year, the gala gave a nod to New York City nightlife with “A New York State of Mind” theme. Party-goers enjoyed live music by the Jazz Loft, dancing, New York-style hor d’oeuvres, casino-style gaming and hand-rolled cigars.
With Jefferson’s Ferry’s “Journey Towards Renewal” renovation and expansion project a hair shy of completion–the new Memory Support Neighborhood is due to open in the coming weeks — the gala honored the two architectural and design firms critical to the project, KDA Architects and Merlino Design Partnership (MDP). Principal architect and KDA Partner David Fowles and principal designer and MDP President Bruce Hurowitz were on hand to accept their honors.
“The outpouring of generosity in support of the Jefferson’s Ferry Foundation and the Resident Assistance Fund is deeply gratifying and demonstrative of the strong community bond we enjoy here at Jefferson’s Ferry,” said President and CEO Bob Caulfield. “We have neighbors helping neighbors through the Resident Assistant Fund and in so many other less tangible but no less important ways. It’s one of the many reasons Jefferson’s Ferry is such a singular community.”
Photo Caption: There was a party going on recently at Jefferson’s Ferry Foundation’s 19th Annual Gala in support of its Resident Assistance Fund, which provides financial assistance to Jefferson’s Ferry residents who outlive their assets or experience a shortfall through no fault of their own. Reflective of this year’s “New York State of Mind” theme, partygoers posed with “NYC taxi cabs” to kick off the event. Pictured here: (L to R:) Jefferson’s Ferry residents Ruth Weinreb, Rose Modica, Josephine Pheffer, Jean Grunwald and Dolores Dellova. (Photo by resident Martin Cohen)
About Jefferson’s Ferry www.jeffersonsferry.org
Jefferson’s Ferry is a not-for-profit Life Plan Community for active adults aged 62 and above, with Independent Living cottages and apartments, assisted living apartments, and a quality health care center all on one site. A multi-million-dollar expansion and renovation project, “The Journey Toward Renewal,” is part of a larger strategic initiative launched in 2018 to create a life-enriching environment for all new and current residents at every stage of their life. Journey to Renewal has added 60 one- and two-bedroom independent living apartments, provided six distinct dining venues, an expanded Healthy Living Center, Fitness Center, and its state-of-the-art Rehabilitation Therapy Center. A new Memory Support Neighborhood will provide a high quality of life and care for people diagnosed and living with Alzheimer’s and other dementia-related diseases. Common areas in Assisted Living and the Health Care Center will be renovated.
Jefferson’s Ferry offers exceptional living and amenities, including indoor pool, computer center, library, recreational areas, gardens, and gazebos. A mix of cultural excursions, civic activities, and a community of residents who help shape Jefferson’s Ferry’s future ensures a spirited and engaged lifestyle.
The Vincent Bove Health Center at Jefferson’s Ferry enjoys a 5-star rating from The Centers for Medicare and Medicaid Services (CMS), and was named a “Best Of” nursing home by U.S. News & World Report. Jefferson’s Ferry has repeatedly earned the industrywide Community Choice Award for resident satisfaction and engagement and has been recognized with the Pinnacle Quality Insight’s Customer Experience Award for five years running. FitchRatings has assigned Jefferson’s Ferry a BBB bond rating. Jefferson’s Ferry has consistently been voted Best Retirement Community, Best Nursing Home and Best Assisted Living on Long Island by The Long Island Press and has been recognized for Excellence by the Hauppauge Industrial Association’s Business Achievement Awards program.
For more information visit www.jeffersonsferry.org
Medical Compass: How can you reduce osteoarthritis pain?
Exercise and diet are keys to improving discomfort
By David Dunaief, M.D.

Osteoarthritis (OA) can make it difficult to perform daily activities and affect your quality of life. It affects the knees, hips and hands most often, and it can disturb your mobility, mood, and sleep quality.
First-line medications can help treat arthritis pain. Acetaminophen and nonsteroidal anti-inflammatory drugs, such as ibuprofen or naproxen are common. Unfortunately, they do have side effects, especially with long-term use. Also, while they might relieve your immediate symptoms of pain and inflammation, they don’t slow osteoarthritis’ progression.
However, you can ease your pain without reaching for medications. Some approaches might even help slow you OA’s progression or reverse your symptoms.
Does losing weight really help with OA pain?
Weight management is a crucial component of any OA pain management strategy. In a study of 112 obese patients, those who lost weight reported that their knee symptoms improved (1). Even more exciting, the study authors observed disease modification, with a reduction in the loss of cartilage volume around the medial tibia. Those who gained weight saw the opposite effect.
The relationship was almost one-to-one; for every one percent of weight lost, there was a 1.2 mm3 preservation of medial tibial cartilage volume, while the opposite occurred when participants gained weight.
A reduction of tibial cartilage is often associated with the need for a knee replacement.
Does increasing vitamin D help reduce OA pain?
In a randomized controlled trial (RCT), vitamin D provided no OA symptom relief, nor any disease-modifying effects (2). This two-year study of almost 150 men and women raised blood levels of vitamin D on average to 36 ng/ml, which is considered respectable. Researchers used MRI and X-rays to track their results.
In another study of 769 participants, ages 50-80, researchers found that low vitamin D levels – below 25 nmol/l led to increased OA knee pain over the five-year study period and hip pain over 2.4 years (3). The researchers postulate that supplementing vitamin D might reduce pain in those who are deficient, but that it will likely have no effect on others.
Does consuming dairy help with OA?
With dairy, specifically milk, there is conflicting information. Some studies show benefits, while others show that it might actually contribute to the inflammation that makes osteoarthritis pain feel worse.
In the Osteoarthritis Initiative study, researchers looked specifically at joint space narrowing that occurs in those with affected knee joints (4). Results showed that low-fat (1 percent) and nonfat milk may slow the progression of osteoarthritis in women. Compared to those who did not drink milk, patients who did saw significantly less narrowing of knee joint space over a 48-month period.
The result curve was interesting, however. For those who drank fewer than three glasses a week up to 10 glasses a week, the progression of joint space narrowing was slowed. However, for those who drank more than 10 glasses per week, there was less benefit. There was no benefit seen in men or with the consumption of higher fat products, such as cheese or yogurt.
However, the study was observational and had significant flaws. First, the 2100 patients were only asked about their milk intake at the study’s start. Second, patients were asked to recall their weekly milk consumption for the previous 12 months before the study began – a challenging task.
On the flip side, a study of almost 39,000 participants from the Melbourne Collaborative Cohort Study found that increases in dairy consumption were associated with increased risk of total hip replacements for men with osteoarthritis (5).
What about yogurt? A published Framingham Offspring Study analysis found that those who consumed yogurt had statistically significant lower levels of interleukin-6 (IL-6), a marker for inflammation, than those who didn’t eat yogurt, but that this was not true with milk or cheese consumption (6).
Would I recommend consuming low-fat or nonfat milk or yogurt? Not necessarily, but I might not dissuade osteoarthritis patients from yogurt.
Which is better, diet or exercise, for reducing OA pain?
Diet and exercise together actually trumped the effects of diet or exercise alone in a well-designed, 18-month study (7). Patients with osteoarthritis of the knee who lost at least 10 percent of their body weight experienced significant functional improvements and a 50 percent pain reduction, as well as inflammation reduction. This was compared to those who lost a lower percent of their body weight.
Researchers used biomarker IL6 to measure inflammation. The diet and exercise group and the diet-only group lost significantly more weight than the exercise-only group, 23.3 pounds and 19.6 pounds versus 4 pounds. The diet portion consisted of a meal replacement shake for breakfast and lunch and then a vegetable-rich, low-fat dinner. Low-calorie meals replaced the shakes after six months. The exercise regimen included one hour of a combination of weight training and walking “with alacrity” three times a week.
To reduce pain and possibly improve your OA, focus on lifestyle modifications. The best effects shown are with weight loss – which is most easily achieved with a vegetable-rich diet and exercise. In terms of low-fat or nonfat milk, the results are controversial, at best. For yogurt, the results suggest it may be beneficial for osteoarthritis, but stay on the low end of consumption, since dairy can increase inflammation.
References:
(1) Ann Rheum Dis. 2015 Jun;74(6):1024-9. (2) JAMA. 2013;309:155-162. (3) Ann. Rheum. Dis. 2014;73:697–703. (4) Arthritis Care Res online. 2014 April 6. (5) J Rheumatol. 2017 Jul;44(7):1066-1070. (6) Nutrients. 2021 Feb 4;13(2):506. (7) JAMA. 2013;310:1263-1273.
Dr. David Dunaief is a speaker, author and local lifestyle medicine physician focusing on the integration of medicine, nutrition, fitness and stress management. For further information, visit www.medicalcompassmd.com or consult your personal physician.
Making Democracy Work: Why Planned Parenthood matters
By Lisa Scott
Nancy Marr’s February 2, 2024 column in this newspaper, “Equal Rights Amendment…It’s Time” explains that the proposed New York State ERA (which will be on the back of the November 2024 ballot) is not “a women’s equality amendment” but seeks to protect women as a class and men as a class against discrimination under the law for any reason. The NYS ERA bill explicitly includes language to clarify that discrimination based on a person’s pregnancy or pregnancy outcomes would be sex discrimination, protecting pregnant people from punishment. These protections will help to guarantee that all people have the right to bodily autonomy.
One organization that has continued to fight to ensure all people have access to the care and resources they need to make informed decisions about their bodies, their lives, and their futures is Planned Parenthood. Planned Parenthood started in 1916 in Brownsville (Brooklyn) New York. In 1933 and 1951, communities in Westchester and Suffolk counties, respectively, were providing health services, accurate information and education, and advocacy for reproductive rights and justice. Today, these counties (with a total population of close to 3 million residents) are now joined as Planned Parenthood Hudson Peconic (PPHP). (All data in this article are as of full-year 2022.)
PPHP now serves as a major provider of sexual and reproductive health care for the region and a leading public advocate in the suburban metro area. There are 10 health centers and 2 mobile health centers, which offer a wide range of sexual and reproductive health care services regardless of the individual’s age, race, ethnicity, religion, gender, sexual orientation, gender identity, immigration status, or ability to pay. In 2022, PPHP provided 45,790 health care visits and served 27,017 patients throughout the 4 counties. Over half of PPHP’s patients are on Medicaid and fall at or below the federal poverty line. Fees for many services are based on a sliding scale tied to income and family size.
PPHP has recently launched initiatives to bring the majority of their health services directly into communities through their mobile health centers, as well as offering expanded telehealth services as an outgrowth of challenges during the COVID pandemic. Reproductive health care cannot wait, so patients can access services such as birth control, emergency contraception, sexually transmitted infection (STI) testing and treatment, HIV testing and education, PrEP and PEP for HIV prevention, gender-affirming care, and more, and access these services with fewer visits or without needing to visit a health center at all.
Every person’s personal decision about their pregnancy should be respected and valued. There is widespread disinformation on Planned Parenthood’s services, in particular abortion services. Contrary to popular belief, abortion is common, nearly one in four women, and more gender expansive people in America will have an abortion by age 45. 6 out of 10 people who get abortions already have kids. PPHP performed 1,993 procedure abortions and 6,238 medication abortions in 2022, but also vasectomies, colposcopies (cervical exams), HPV vaccinations, breast exams, and pap tests. STI tests (59,530) and contraception management visits (33,199) were by far the service most in demand/provided.
PPHP is one of eight Planned Parenthood affiliates to offer prenatal care. The organization recently launched Centering Pregnancy in two of its health centers, an innovative style of group prenatal care that empowers pregnant people to be actively involved in their own care and equips them to make healthy choices throughout their pregnancy and beyond. Numerous published studies show that Centering patients have healthier babies and that Centering nearly eliminates racial disparities in preterm birth. PPHP is committed to improving maternal health outcomes and reducing maternal mortality, particularly among people of color.
We should be empowering people to make their own health and reproductive care decisions, and remind them that there is a team of health professionals at PPHP that can answer questions and address concerns with understanding and respect. And voting yes in November for the NYS ERA will take a big step to protecting a person’s right to make decisions about their own bodies. PPHP can be reached at 800-230-PLAN or visit pphp.org.
Lisa Scott is president of the League of Women Voters of Suffolk County a nonprofit, nonpartisan organization that encourages the informed and active participation of citizens in government and influences public policy through education and advocacy. For more information, visit https//my.lwv.org/new-york/suffolk-county.
Ahead in removing forever chemicals, NYS preps for higher drinking water standards

By Daniel Dunaief
Forever is wonderful when it comes to love, but not so much when it comes to chemicals that don’t break down and stay in the human body, accumulating over time and threatening people’s health.
In a move applauded by environmental advocates and health officials, the Environmental Protection Agency last week set a limit on the amount of so-called forever chemicals, such as per- and polyfluoroalkyl substances, called PFAS, of four parts per trillion in drinking water.
Water companies have until 2027 to complete initial monitoring to reduce chemicals that have been linked to damage to the kidney, testes, liver, thyroid, reproductive and immune system, according to the new regulations. Found in a host of products including fireman’s foam, carpets, clothing, food packaging and nonstick cookware, PFAS are resistant to oil and water.
New York State already had one of the toughest regulations in the country, as the Empire State set maximum contaminant levels of 10 parts per trillion for these chemicals in 2020.
Charles Lefkowitz, chairman of the Suffolk County Water Authority applauded the EPA for this new national standard.
The SCWA has been “preparing for this and we are well on our way to meeting all regulatory requirements within the time frame laid out by EPA,” Lefkowitz said in a statement. “Since 2020, when New York enacted its own PFAS rules, SCWA has been meeting or surpassing all standards. It has given us a great head start on the new rules, but there is still work to be done.”
Suffolk County Health Commissioner Dr. Gregson Pigott noted that the state’s water standards for emerging contaminants are among the most protective in the country.
“The new federal measures will have the greatest impact nationwide and will also further protect our drinking water on Long Island,” Dr. Pigott explained in an email.
Environmental groups recognized the ongoing work at the SCWA to meet these standards and appreciated the authority’s public disclosure of its testing results.
Adrienne Esposito, Executive Director of Citizens Campaign for the Environment, described the SCWA as “ready” for this rule change and “poised for action.”
Since 2016, the SCWA installed 27 new Granular Activated Carbon treatment systems that remove PFAS from drinking water, The authority expects to install as many as 80 new GAC systems to meet the new regulations.
“We are well within our way to achieving that within the timeframe set by the EPA,” Jeff Szabo, Chief Executive Officer of SCWA, explained in an email.
Each new system costs about $1.5 million to install. SCWA had already instituted a $20 per quarter water quality treatment charge to customers in 2020, when New York State established its PFAS limits.
SCWA has also secured $9 million from New York State for GAC treatment, which, Szabo explained, would help reduce the cost to customers.
Rates won’t be increasing in the next fiscal year. The rates, which are based on the budget, may change in future years, depending on the operating budget, a spokesman said.
SCWA tests all of its wells at least semi-annually for PFAS. If the authority finds a well with these chemicals, it retests the well at least quarterly and, in some cases will test it every month or every two weeks.
Private wells
Esposito urged people with private wells to test their water regularly.
“People think when they have a private well, it comes from a mysteriously clean spring,” said Esposito. “They must get their wells tested. Ignorance is not bliss. If there are PFAS, they must call and report it and see if they’re eligible to get federal funds for filtration.”
Esposito estimates the cost of testing for private well water could be $200 to $250.
Carbon filtration, using a process called reverse osmosis, can remove PFAS.
The cost of installing filters depends on the home and the type of filter. Several online providers estimate a cost between $800 and $3,000, although specific costs from different providers may vary.
Residents can call the Department of Health Services Office of Water Resources at (631) 852-5810 for information on testing by either the health department or a local contract laboratory. Health department staff are also available to provide treatment recommendations.
The New York State Department of Environmental Conservation has provided alternate water supplies to a limited number of private well owners on a case-by-case basis over the last several years.
The New York State legislature is considering proposed legislation to provide grant funding to private well owners with impacted wells to connect to public water or install treatment.
The county health department coordinates with the DEC and the state Department of Health when they receive information regarding water that exceeds PFAS containment levels.
People interested in further information about the health effects of the PFAS are urged to reach out to the New York State Department of Health.
Jaymie Meliker, Professor in the Department of Family, Population and Preventive Medicine in the Program in Public Health at Stony Brook University, added that private wells have numerous potential contaminants in part because Long Island has so many septic systems.
These wastewater systems are a source of nitrogen for waterways, leading to fish kills and can also add contaminants to drinking water.
Wastewater treatment is “vastly under resourced,” said Meliker. The county and the state need infrastructure investments.
As for PFAS, they can vary from one neighborhood to the next.
On the manufacturing side, companies are working to lower the toxins of PFAS, creating shorter chains that provide the same benefits without the negative effect on health.
Meliker was pleased that the EPA had established low level limits for these chemicals that accumulate in the human body.
The studies and concerns have been “going on for a couple of decades,” he said. “There’s enough evidence to suggest it’s prudent to do something.