Phew!
The dramatic and steep rise in positive infections caused by the ubiquitous omicron mutant of the original COVID-19 strain is declining almost as rapidly as it climbed.
As of Tuesday, Jan. 25, the seven-day average for the percentage of people who tested positive for COVID in Suffolk County stood at 12%, which is well below the 25.9% for the same seven-day average who tested positive just two weeks earlier, according to figures from the New York State Department of Health.
Those numbers, which have been declining on a daily basis, are likely to fall even further, experts said.
“The omicron wave appears to have crested in Suffolk County and New York State, but not in other parts of the country,” Dr. Gregson Pigott, commissioner of the Suffolk County Department of Health Services, wrote in an email.
Public health officials attribute the welcome decline to several factors, including the increasing use of boosters, the adherence to mask guidelines and the reduction in travel and group gatherings.
“The numbers will decline slowly and steadily from the teens to single digits,” said Dr. Sunil Dhuper, chief medical officer at Port Jefferson’s St. Charles Hospital.
Sean Clouston, associate professor in the Program in Public Health and the Department of Family, Population and Preventive Medicine at the Renaissance School of Medicine at Stony Brook University, added in an email that the “decline appears real and the timing suggest that the holiday period was, again, the main driving factor in the higher rates. We are likely on the other side of this wave.”
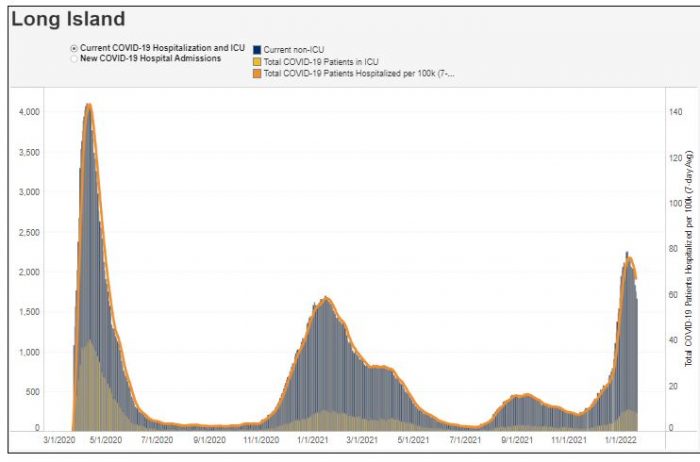
The omicron variant, which has involved milder symptoms for many of those infected, has also resulted in fewer hospitalizations.
The increase in hospitalizations is “not proportionate to the rise in cases” Pigott explained. “Our hospitals were overwhelmed when SARS-CoV-2 first hit our area [in 2020]. That has not been the case for the delta wave or the omicron wave.”
Indeed, the increase in the percentage of people who are vaccinated and boosted has helped reduce the need for emergency medical services at hospitals.
Among fully vaccinated people in the state of New York, 0.23% of the population 12 and over has been hospitalized, according to the New York State Department of Health.
That trend also holds true in Suffolk County area hospitals, public health officials said.
“We are seeing significantly reduced number of adults admitted with COVID who have had vaccines and especially those who had vaccines plus boosters,” Dr. Sharon Nachman, chief of the Division of Pediatric Infectious Diseases at Stony Brook Children’s Hospital, explained in an email. “We suspect that the booster augments your initial immune response, lasting at least six months.”
While vaccines and boosters help prevent hospitalizations, they do not ward off all potential upper respiratory infections, Nachman added. Getting a primary series and a booster is “critical” to reducing the risk of more significant health effects from any potential infection.
The age range of people who are hospitalized has decreased, particularly during the third wave. In the first exposure to the Wuhan strain, a majority of those who needed critical medical care were over 65, particularly before the vaccine was available.
During the omicron wave, however, there is a “noticeable shift between the ages of 18 to 49,” Dhuper said. While the proportion of people as a whole in this group may be lower, in part because people in this age range may not have as many underlying medical conditions, the total number hospitalized is still higher because of the broader spread of the virus.
People in that younger age bracket are “the major shift,” Dhuper said.
The infectiousness of omicron also created a strain on hospitals, as health care workers, even those who were asymptomatic or had minor symptoms, were testing positive.
“We had never seen the number of staff members that were out during the first or second wave,” Dhuper said. Even though the number of people hospitalized wasn’t as high, the overall health care workers available to help care for the population “really stressed our system.”
In the prior waves of the pandemic, the Catholic hospitals were able to do load balancing, in which they shifted patients to hospitals that had the bed space and health care workers.
Toward the latter half of the omicron wave, such maneuvers weren’t as easy to manage in part because of the staff shortages caused by positive tests.
Discharging people earlier and using effective but limited supply monoclonal antibody treatments for eligible patients that reduce the severity of symptoms helped reduce the strain on the system, Dhuper added.
In terms of protecting the population, Dhuper urged residents to consider the benefit of vaccines and boosters.
“The majority of patients hospitalized in the intensive care unit are unvaccinated,” Dhuper said.
The rate of people who were unvaccinated and hospitalized with COVID-19 in the week ending on Dec. 11, which was the highest figure for 2021, was 91.1 per 100,000 people in the population, compared with 4.1 per 100,000 among the vaccinated, according to the New York State Department of Health.
“Those are amazing numbers in terms of the role of vaccines and how it’s protecting people from getting hospitalized and dying,” Dhuper said.