In Suffolk County, the number of positive COVID-19 tests has been steadily climbing in the last month, mirroring the increase in other counties in the state and in parts of the country.
As of May 9, the number of people who tested positive per 100,000 residents on a seven-day average was 47.8. That is up from 34.9 a week earlier, 13.4 on April 9 and 6.3 on March 8, just over two months earlier, according to data from the New York State Department of Health.
“The numbers are creeping up,” said Dr. Mickel Khlat, chief medical officer at St. Catherine of Siena Hospital in Smithtown. Catholic Health had about 28 to 30 patients a month ago with COVID-19 and that number has now risen to the mid-60s. Most of those are incidental, he added, as the hospital discovered a positive test when a patient came in for another procedure. These positive tests, however, reveal the ongoing presence of the virus in the community. “I was hoping in 2022 that this would go away, but I don’t see this going away any time soon.”
Area doctors and health officials suggested familiar practices to reduce risks, including social distancing and mask-wearing in confined spaces indoors and ensuring up-to-date vaccinations.
“Immunity from vaccines and immunity from infection with SARS-CoV-2 virus wanes, so we urge everyone to get vaccinated and to get their booster or second booster if you are eligible,” Dr. Gregson Pigott, commissioner of the Suffolk County Department of Health Service, explained in an email.
Dr. Sharon Nachman, chief of the Division of Pediatric Infectious Diseases at Stony Brook Children’s Hospital, suggested that the hospital is recommending that people speak to their primary care providers to get the best advice on their need to get a second booster.
“Often, individuals may not realize that they fall into a category of vulnerable populations,” she explained in an email. “These can include not only adults with immune issues, but also those with heart and lung diseases, kidney issues, obese individuals and, of course, those who are elderly.”
Khlat said since the virus first reached Suffolk County, obesity is often the underlying condition that presents the greatest risk factor for dying, which was evident in the first and second surges.
People of all ages in Suffolk County have been hospitalized, even children, Pigott added.
Recently, fewer sick people have needed medical attention in the intensive care unit.
The majority of people who are under 65 years old and in the ICU are unvaccinated, Pigott added.
In general, the most common symptoms for COVID-19 include respiratory issues as well as fever, Nachman said. Other symptoms include gastrointestinal issues.
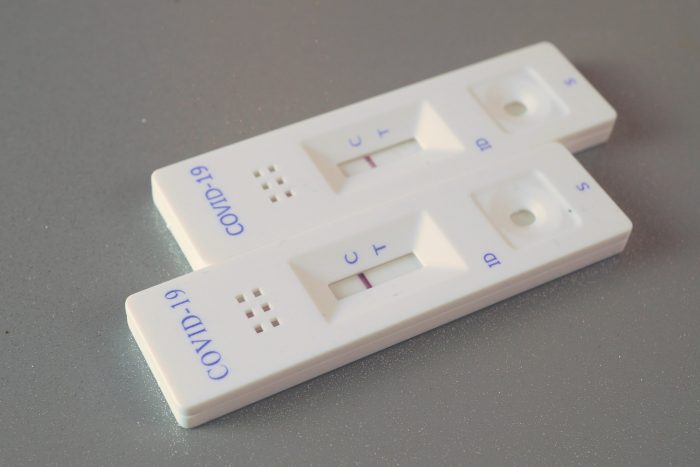
“If you have symptoms, please consider doing a rapid test to evaluate the possibility” of having the virus, Nachman added.
The coming fall and winter
In the broader context, state and national officials are anticipating a challenging fall and winter. Earlier this week, the White House estimated that the country could experience as many as 100 million new infections without renewed mitigation measures.
While daunting, particularly in the third year of the pandemic, the large number of potential new infections could encourage Congress to appropriate more funds to combat the virus and alert state officials to the need for measures to protect residents.
Area hospitals have already started to consider the possibility of a rise in infections later this year.
“We are anticipating increase in illness this upcoming fall and winter and are addressing those needs now” through supply chain preparations and other measures, explained Nachman.
Khlat said St. Catherine continues to make sure the hospital has enough personal protective equipment, including N95 masks. While he suspects the tighter quarters in colder weather could contribute to a surge, he doesn’t expect people will be as sick this time.
If they do get sick, patients can receive the first and second dose of remdesivir in the hospital and then get their next few doses at home, through a hospital-at-home program.
Medical options
Pigott urged those who are at risk and test positive to contact their medical providers soon after testing positive and/or developing symptoms.
Those who contract COVID-19 have several therapeutic options, especially if they have mild-to-moderate symptoms and are at risk for severe disease.
“COVID-19 antiviral medications or therapies should be started within five to seven days of symptom onset,” Pigott explained.
Nachman added that treatments for Covid include monoclonal antibodies and Paxlovid.
“They can be difficult to get, difficult to take and, particularly for Paxlovid, have serious drug-drug interactions,” Nachman cautioned. “They are indicated for those with underlying medical issues. Other therapies, although less commonly available, include intravenous remdesivir.”
Khlat said he’d recently heard of two cases in which patients took a five-day course of Paxlovid.
“A week or two later, they came back for monoclonal antibodies,” he said. People had “relapsed from Paxlovid. That, I never heard of before.”
Generally, Khlat said Paxlovid works well, although he, too, cautioned about drug interactions.
With fewer and shorter hospital stays for people who contract COVID-19, hospitals continue to have capacity. “We are not seeing an influx of patients getting admitted for COVID,” Khlat said.











 “Supervisor Wehrheim has been an example of the kind of leadership that you need in unprecedented times, and I truly appreciate his partnership and the work that we were able to do together during the pandemic,” Bellone said.
“Supervisor Wehrheim has been an example of the kind of leadership that you need in unprecedented times, and I truly appreciate his partnership and the work that we were able to do together during the pandemic,” Bellone said.