Suffolk County’s positive COVID-19 tests continue to decline
Over the last month, the pandemic trends continue to improve in Suffolk County and in the country.
After a rocky start to the New Year, brought on by an omicron variant that was more contagious than either the original strain of the virus or the delta variant, the percentage of positive tests in Suffolk County continues to decline.
As of Feb. 7, the percentage of positive tests over a seven-day average in Suffolk County was 4.9%, according to the New York State Department of Health. That is down from 14% on Jan. 21 and 27% on Jan. 7.
The trends on Long Island are following similar patterns in other parts of the world that experienced the omicron infection earlier.
South Africa “experienced the omicron wave first,” Dr. Gregson Pigott, health commissioner of the Suffolk County Department of Health Services, wrote in an email. “Almost as steeply as cases rose, they fell.”
Indeed, at Port Jefferson’s St. Charles Hospital, Dr. Sunil Dhuper, chief medical officer, said there has been a “significant” drop in the number of patients hospitalized and in the number of Emergency Room visits, while the use of monoclonal antibodies to treat patients in the early stages of an infection has also dropped dramatically.
“We are not seeing the kind of volume we were seeing a few weeks ago,” Dhuper added.
The Department of Health for the country reported that the reinfection rate, which reached a peak in the last week of December and first week of January, has also been declining.
The number of hospitalizations throughout the country has fallen enough that Dr. Anthony Fauci, the chief medical adviser to President Joseph Biden (D), recently said in an interview with the Financial Times that the country is almost past the “full-blown” pandemic phase. While he didn’t offer a specific timetable, he suggested that virus restrictions could be lifted within a matter of months.
Area doctors suggested that vaccinations and more mild symptoms among those who contracted the virus helped alleviate the strain on the health care community.
“The vast majority of those hospitalized for respiratory or other COVID-type illnesses have not been vaccinated,” Dr. Sharon Nachman, chief of the Division of Pediatric Infectious Diseases at Stony Brook Children’s Hospital, explained in an email.
While the overall number continues to decline, the county, and the country, need to make continued progress in reducing the overall infection rate before the all-clear signal.
Sean Clouston, associate professor in the Program in Public Health and the Department of Family, Population and Preventive Medicine at the Renaissance School of Medicine at Stony Brook University, suggested that the current number of infections still leaves room for improvement.
A positivity rate above 5% which was the figure earlier this week, is “still extremely high,” Clouston explained in an email. “Currently, the [Centers for Disease Control and Prevention] would recommend that no one in the globe travel to Long Island, which doesn’t seem like we ourselves see this as safe objectively.”
Health care providers highlighted the difference between the reported and the actual infection numbers.
When the pandemic started in March of 2020, Dhuper estimates that the ratio of reported to actual cases was close to 1 to 10. With Delta, that number likely dropped to closer to 1 to 5, and with omicron, that’s probably about 1 to 3 or 4.
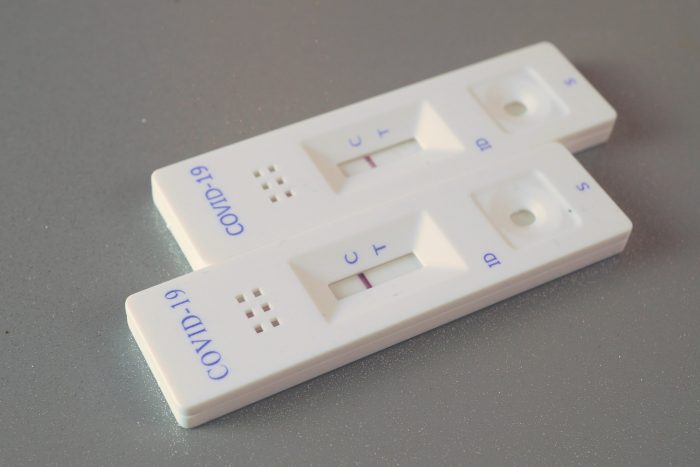
With the increase in at-home testing, the numbers “we see are more of a sampling, showing the approximate prevalence of COVID-19 virus circulating in the population,” Pigott explained.
Nachman added that Stony Brook is following guidelines from the Food and Drug Administration and the Centers for Disease Control and Prevention when it comes to vaccinations for people who tested positive for COVID-19.
These public health authorities generally recommend a booster dose after people feel well, which is usually 10 days to two weeks after an illness.
Doctors said they are monitoring a new version of the omicron variant, called BA.2
The new variant seems a “bit more” contagious” than the original omicron, Dhuper said. Vaccines, however, have a “reasonable level of protection to prevent hospitalizations and death.”
Dhuper said he continues to “keep an eye” on that variant.
Nachman suggested that the available vaccines continue to help.
“Right now, the [two omicron variants] do not seem to be radically different,” she suggested, as both have a short incubation period and people are protected by the vaccine.
With the number of people contracting the virus and developing more severe symptoms declining, Dhuper said the demand for the effective monoclonal antibody treatment continues to fall.
Dhuper said a recent New England Journal of Medicine study indicated that the antiviral treatment remdesivir, manufactured by Gilead Sciences, was effective at treating mild to moderate illnesses on an outpatient basis over a three-day period.
“Given under controlled conditions, (remdesivir) could be one of the best alternatives that we have,” Dhuper said.