Joel Gonzalez was waking up in the middle of the night, gasping for air. During the day, if he ate too quickly, he felt like food was getting stuck in his throat.
In 2018, Gonzalez, who lives in Coram and is a high school counselor, was diagnosed with gastroesophageal reflux disease, or GERD. A small hiatal hernia, in which part of his stomach bulged through an opening in his diaphragm and into his chest, caused the condition.
Gonzalez started taking medications, which helped relieve the symptoms and enabled him to sleep without experiencing discomfort or waking up suddenly.
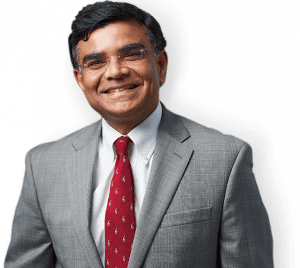
In August 2022, after learning that his hiatal hernia had gotten slightly larger and deciding he didn’t want to continue taking reflux medicine for the rest of his life, he met with Dr. Arif Ahmad, director of the St. Charles and St. Catherine of Siena Acid Reflux and Hiatal Hernia Centers of Excellence, to discuss the possibility of surgery.
Gonzalez was so convinced that the surgery would help and confident in Dr. Ahmad’s experience that he scheduled the procedure during that first meeting. Since his November surgery, which took about an hour, he hasn’t had any GERD symptoms and is not taking any medication for the condition.
Gonzalez said he would “absolutely” recommend the surgical procedure, which became a “simple decision” after consulting with Dr. Ahmad.
Caused by a mechanical problem with a valve at the bottom of the esophagus called the lower esophageal sphincter that allows stomach acid to enter the esophagus, GERD affects over 20% of the population.
Symptoms of GERD vary, which means doctors can and do take a range of approaches to treatment.
Hospitals, including St. Charles, St. Catherine of Siena, Stony Brook and Huntington Hospital, have been ramping up their efforts to evaluate and treat GERD.
Port Jefferson-based St. Charles and Smithtown-based St. Catherine of Siena, both part of the Catholic Health system, have been expanding these services at the Acid Reflux and Hiatal Hernia Centers of Excellence.
“There is a big need” for this increasingly focused effort to help patients dealing with the symptoms of GERD, said Dr. Ahmad.
At St. Charles and St. Catherine, Dr. Ahmad, who has been doing hiatal hernia and GERD-correcting surgery for over 25 years, created the center to ensure that the nurses on the floor, the people who do the testing, and the recovery staff are aware of the specific needs of these patients.
Dr. Ahmad has done presentations for the staff to ensure they have “the highest level of expertise,” he added.
Dr. Ahmad, also the director of the Center of Excellence in Metabolic and Bariatric Surgery at Mather Hospital, said he could perform surgery, if a patient needs it, at any of the hospitals, depending on a patient’s request.
Stony Brook’s efforts
At the same time, Stony Brook recently created a multidisciplinary Esophageal Center at Stony Brook Medicine, designed to provide a collaborative care model for diagnosing and treating GERD.
The center provides minimally invasive endoscopic treatments as well as surgical options.
Dr. Lionel D’Souza, chief of endoscopy, said the center provides a cohesiveness that “allows an evaluation by a group of people who are experts and can communicate with each other” to provide a patient-specific plan.
Dr. D’Souza suggested people seek medical attention from their primary care physician or gastroenterologist if they experience any of the following conditions: heartburn every day or severe heartburn several times a week, trouble swallowing, food getting stuck in the throat, anemia, blood in the stool or weight loss without another explanation.
Other partners in the Stony Brook GERD Center include Dr. Olga Aroniadis, chief of the division of gastroenterology, Dr. Alexandra Guillaume, director of the gastrointestinal motility center, and Dr. Konstantinos Spaniolas, chief of the division of bariatric, foregut and advanced GI surgery at Stony Brook Medicine and director of Stony Brook’s bariatric and metabolic weight loss center.
“When someone has a lot of excess weight, the chance of developing GERD is a lot higher,” Dr. Spaniolas said. “Sometimes, getting patients through a program to facilitate with weight loss can help [people] avoid GI symptoms, such as heartburn.”
Stony Brook will see patients in different parts of its network and then, depending on the needs, will determine who is best-suited to start their work up and treatment, Dr. Spaniolas added.
While a potential option, surgery is among a host of choices for people who have ongoing heartburn.
Huntington Hospital, meanwhile, will begin offering esophageal motility testing starting in June. Patients can call Northwell Health’s Heartburn and Reflux Center to schedule an appointment.
A team of gastroenterologists, surgeons and dietitians will work with patients at Huntington to determine the cause of GERD and possible treatments, according to Dr. David Purow, chief of gastroenterology.
Soft foods
Those who have surgery return to solid foods gradually.
Marlene Cross, a resident of St. James who struggled with GERD for about a decade, had the procedure in March.
For the first few weeks, she ate primarily liquids, with some protein drinks and puddings. She added Farina and oatmeal to her diet and then could eat flaky fish.
At 83, Cross, who lost sleep because of GERD-induced heartburn, said the surgery was a success.
“I’m not running a marathon, but I’m definitely feeling a lot better,” said Cross, who is a retired teacher’s assistant for special education students.
Cross urged others who might benefit from surgery to “see a specialist and ask questions and do it” if the doctor recommends it. “The younger you do it, the better.”