Wednesday, Aug. 9, is an important deadline for veterans who were exposed to burn pits.
That is the cutoff point when veterans can file claims for health issues that date back to the passage of the PACT Act in August 2022. If they file paperwork by Wednesday, they can get retroactive benefits.
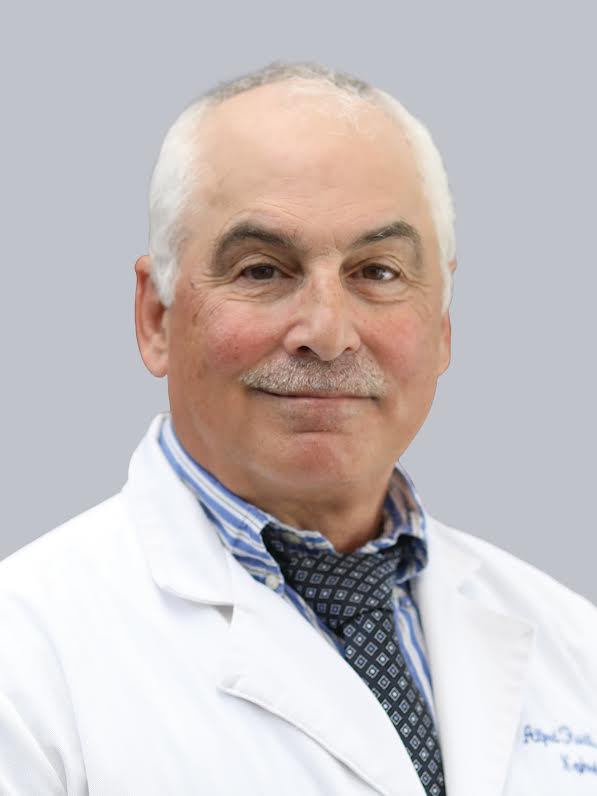
“It’s very important” that veterans who might have health-related problems file for these benefits before that deadline, said Dr. Anthony Szema, director of the International Center of Excellence in Deployment Health and Medical Geosciences, Northwell Health Foundation.
A veteran filing after Aug. 9 may only qualify for prospective medical care.
“The sooner you apply, the more benefits you may be eligible for,” explained Fernando X. Burgos Ortiz, Public Affairs Officer at the Northport VA Medical Center.
If veterans apply for PACT-related benefits on or before August 9, their benefits may be backdated to August 10, 2022.
People who are not ready to submit a full claim by then can also submit a quick “intent to file” and still receive the effective date, explained Burgos Ortiz. Veterans and survivors can visit va.gov/PACT to apply or submit their intent to file through the link: Your intent to file a VA claim | Veterans Affairs.
Veterans who apply after Aug. 10 may still be eligible to have their benefits backdated by one year, if they would have been eligible for PACT benefits on Aug. 10, 2022. A veteran who applied in December 2025 could have their benefits, if granted, backdated to December 2024. In that case, however, they would miss out on the earliest possible effective date of Aug. 10, 2022, which would mean they would miss out on a couple of years of benefits, Burgos Ortiz wrote.
‘You got exposed to a ticking time bomb, and we need to defuse it now so it never becomes a problem.’ — Dr. Anthony Szema
With support from numerous veteran advocates, including comedian John Stewart, Burn Pits 360 and others, Congress passed the PACT Act last August to ensure that veterans exposed to toxins from particles aerosolized by burn pits received ongoing medical support.
Szema, who specializes in asthma and lung fibrosis, urged all veterans who might qualify for these benefits to call their local VA and ask how to file for PACT Act benefits.
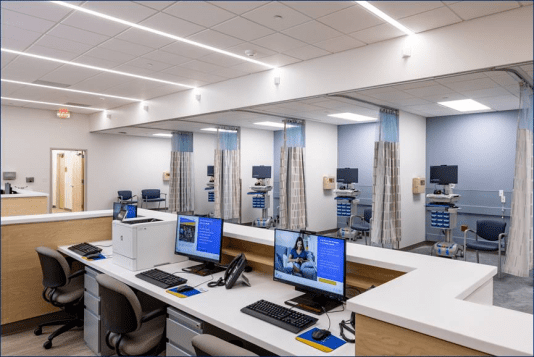
Through its offices on 3771 Nesconset Highway in Suite 105 in South Setauket, Northwell Health provides special testing to confirm the potential health effects of this exposure.
Last week, two veterans had such evaluations, while three signed up for Tuesday.
Conditions covered on the list include a wide range of health issues, including brain cancer, any type of gastrointestinal cancer, glioblastoma, head cancer, kidney cancer, lymphoma of any type, melanoma, neck cancer of any type, pancreatic cancer, reproductive cancer and respiratory cancer.
Covered conditions also include asthma, chronic bronchitis, COPD, emphysema, granulomatous disease, interstitial lung disease, pleuritis, pulmonary fibrosis and sarcoidosis.
Around the country, 2.5 million vets could receive benefits, including 8,000 in the greater New York Metropolitan area, Szema said.
“Thousands of vets are unaware” of the deadline, he added.
Prior to the PACT Act, Szema said the VA denied about 80% of claims. Now, presumptive conditions are covered rather than on a case-by-case basis.
Szema suggested that many veterans who breathed the air around burn pits and were living in dusty environments in Iraq and Afghanistan could be asymptomatic today, but might already be headed toward future health crises.
“If you believe [people who lived near the] World Trade Center have disease, this is worse, because you live 300 yards away from trash being burned with jet fuel in open air,” he said.
Szema said the tests Northwell conducts provide a more accurate reading of potential breathing or allergic problems in a shorter time. Northwell uses pulmoscan impulse oscillometry, in addition to respiratory muscle strength and multi test percutaneous allergy testing with plastic, which doesn’t involve needles.
Northwell has 10 remote patient monitoring systems from Bodimetrics that allows them to monitor continuous oxygen saturation and heart rate variability of veterans. The information also goes to the smart phones of veterans and to a remote modeling team with a nurse and to a cardio thoracic surgeon in Kansas.
Northwell is in discussions to obtain more of these systems.
Szema recently published a paper indicating that 29% of veterans exposed to burn pits reported seeing blood in their urine. Exposure to benzene and naphthalene in JP-8 jet fuel poses a risk of bladder cancer.
“It is never normal to have blood in the urine, even if it is kidney stones,” Szema wrote in an email. “Since these veterans were exposed to carcinogens, a thorough evaluation is paramount.”
Szema added that soldiers who answered the call of duty may not have symptoms but could develop them in the coming years.
“You got exposed to a ticking time bomb, and we need to defuse it now so it never becomes a problem,” he said.
Developing awareness
Szema was chief of the allergy section of Veterans Affairs Medical Center at Northport between 1998 and 2015. Between 1998 and 2004, his patients were primarily 80-year old Caucasian men who were in wheelchairs and needed oxygen.
All of a sudden, in September 2004, he and a medical student and “everybody was 20 years old in uniform” with patients who were brown, African American, black, hispanic, Southeastern Asian and Native American, reflecting the “entire diversity of Long Island.”
An index case of an all-state football player raised his level of concern, as the athlete didn’t smoke, vape or smoke marijuana but had shortness of breath.
At first, Szema thought his physical problems came from inhaling dust from storms. That prompted him to initiate his first study reporting asthma among veterans returning from deployment to Iraq and Afghanistan near burn pits.
Szema testified before the United States Senate Policy Committee in Washington, D.C. in 2009.
He urged veterans who think they might qualify for these benefits to reach out to Three Village Asthma in South Setauket at 631-675-6474. The office is across the street from Jefferson Ferry.
“Now is the time,” Szema said. “At least if you get diagnosed with a condition related to your exposure, you can receive timely treatment.”