On Monday Aug. 7 the St. James Fire Department, 533 North Country Road, St. James will host a community blood drive from 2 to 8 p.m. Walk-ins are welcome. Come help address the critical blood shortage and do your part to save a life. For more information, call the fire department at 631-584-5760 or New York Blood Center at 1-800-933-2566.
Medical Compass: Americans are woefully deficient in critical nutrients
We know better. So why can’t we do better?
By David Dunaief, M.D.

We are continuously inundated with messages about the importance of including fruits and vegetables in our daily diets. In addition to fiber, they include critical nutrients and micronutrients that keep us healthy and reduce our risks of developing chronic diseases.
Despite this, according to a 2022 report by the Centers for Disease Control and Prevention (CDC), an average of 12.3 percent of U.S. adults met the daily requirements for fruit intake, and an even more abysmal 10 percent met vegetable intake recommendations (1). As you might expect, it follows that we are deficient in many key micronutrients (2).
Why do we care? Most chronic diseases, including common killers, such as heart disease, stroke, diabetes and some cancers, can potentially be prevented, modified and even reversed with a focus on nutrients.
Here’s a stunning statistic: more than 50 percent of American adults have a chronic disease, with 27 percent having more than one (3). This is likely a factor in the slowing pace of life expectancy increases in the U.S., which have plateaued in the past decade and are currently at around 77 years old.
One indicator of nutrient intake that we can measure is carotenoid levels. Carotenoids are nutrients that are incredibly important for tissue and organ health. I measure these regularly, because they give me a sense of whether the patient might lack potentially disease-fighting nutrients. A high nutrient intake dietary approach can resolve the situation and increase both carotenoid and other critical nutrient levels.
Why focus on a high nutrient intake diet?
A high nutrient intake diet focuses on micronutrients, which literally means small nutrients, including antioxidants and phytochemicals — plant nutrients. Micronutrients are bioactive compounds found mostly in foods and in some supplements. While fiber is not considered a micronutrient, it also has significant disease modifying effects. Micronutrients interact with each other in synergistic ways, meaning the sum of them is greater than their parts. Diets that are plant-rich raise the levels of micronutrients considerably in patients.
In a 2017 study that included 73,700 men and women who were participants in the Nurses’ Health Study and the Health Professionals Follow-up Study, participants’ diets were rated over a 12-year period using three established dietary scores: the Alternate Healthy Eating Index–2010 score, the Alternate Mediterranean Diet score, and the Dietary Approaches to Stop Hypertension (DASH) diet score (4).
A 20 percent increase in diet scores, which indicated an improved quality of diet, was significantly associated with a reduction in total mortality of 8 to 17 percent, depending on whether two or three scoring methods were used. Participants who maintained a high-quality diet over a 12-year period reduced their risk of death by 9 to 14 percent more than participants with consistently low diet scores over time. By contrast, worsening diet quality over 12 years was associated with an increase in mortality of 6 to 12 percent. Not surprisingly, longer periods of healthy eating had a greater effect than shorter periods.
This study reinforces the findings of the Greek EPIC trial, a large, prospective cohort study, where the Mediterranean-type diet decreased mortality significantly — the better the compliance, the greater the effect (5). The most powerful dietary components were the fruits, vegetables, nuts, olive oil, legumes and moderate alcohol intake. Low consumption of meat also contributed to the beneficial effects. Dairy and cereals had a neutral or minimal effect.
How can diet improve your quality of life?
Quality of life is as important as longevity. Let’s examine some studies that consider the impact of diet on diseases that may reduce our quality of life as we age.
A study showed olive oil reduces the risk of stroke by 41 percent (6). The authors attribute this effect, at least partially, to oleic acid, a bioactive compound found in olive oil. While olive oil is important, I recommend limiting olive oil to one tablespoon a day. Each tablespoon of olive oil contains 120 calories, all of them fat. If you eat too much of even good fat, it can be counterproductive. The authors commented that the Mediterranean-type diet had only recently been used in trials with neurologic diseases and results suggest benefits in several disorders, such as Alzheimer’s.
In a case-control study that compared those with and without disease, high intake of antioxidants from food was associated with a significant decrease in the risk of early Age-related Macular Degeneration (AMD), the leading cause of blindness in those 55 years or older (7). This was true even when participants had a genetic predisposition for the disease.
There were 2,167 people enrolled in the study with several different genetic variations that made them high risk for AMD. Those with a highest nutrient intake, including B-carotene, zinc, lutein, zeaxanthin, EPA and DHA- substances found in fish, had an inverse relationship with risk of early AMD. Nutrients, thus, may play a role in modifying gene expression.
Though many Americans are malnourished, nutrients that are effective and available can improve our outcomes. With a focus on a high nutrient intake diet, we can improve life expectancy and, on an individual level, improve our quality of life.
References:
(1) cdc.gov. Morb Mortal Wkly Rep 2022;71:1–9. (2) cdc.gov/nutritionreport (3) cdc.gov. (4) N Engl J Med 2017; 377:143-153. (5) BMJ. 2009;338:b2337. (6) Neurology June 15, 2011. (7) Arch Ophthalmol. 2011;129(6):758-766.
Dr. David Dunaief is a speaker, author and local lifestyle medicine physician focusing on the integration of medicine, nutrition, fitness and stress management. For further information, visit www.medicalcompassmd.com or consult your personal physician.
Shed the Meds event heads to Emma Clark Library
Emma Clark Library, 120 Main St., Setauket presents a Shed the Meds event on Tuesday, Aug. 8 from 4 to 7 p.m. The Suffolk County Sheriff’s Office hosts this safe way to properly dispose of unused medications. Proper disposal is essential to protect the environment and ensure that old drugs don’t end up in the wrong hands. Please note: The Suffolk County Sheriff’s Office cannot accept any liquids, needles, creams, or ointments of any kind. They are only accepting unused or expired medications from individuals (not large quantities from a doctor’s office or health care facility). Questions? Email [email protected]
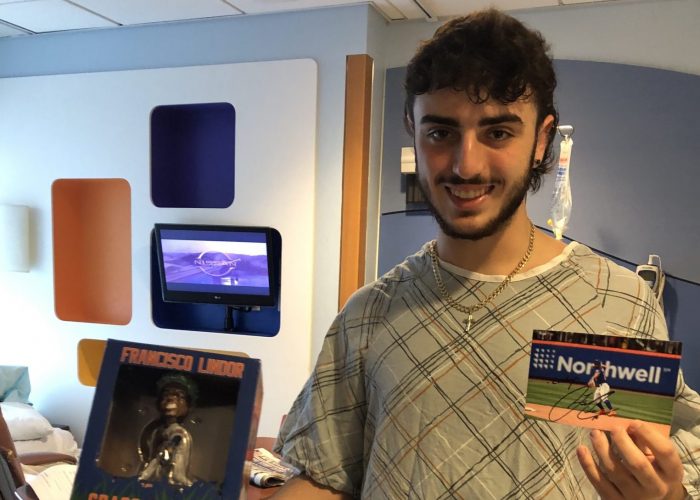
GoFundMe organizers seek to ‘attack’ medical bills for John Glenn student
By Rita J. Egan
Friends are rallying around an Elwood-John H. Glenn High School student to raise money for his medical treatment.
In July, doctors diagnosed high school senior Zach Berger with Ewing sarcoma, a rare and aggressive pediatric cancer. As soon as they heard the news, his mother’s friends, Carolyn O’Brien and Courtney Presti, along with Berger’s friend and O’Brien’s son Joseph Pontieri, set up a GoFundMe page to raise $50,000 to help offset medical costs and ease financial strains.
Berger’s mother, Dinah, said his family, which includes his dad David and older sister Katrina, was surprised and touched when they heard about the GoFundMe campaign.

In addition to donations, Berger’s friends and their families have been showing their support in various ways. His mother said a friend’s father who owns a diner has regularly brought them food since he heard the news.
“We have a saying, ‘Elwood Strong,’ and they’ve really proven it,” Dinah Berger said, adding she couldn’t thank the community enough.
The fundraising campaign organizers are using the hashtag #elwoodstrong as well as #zachattack, which O’Brien said has been used when Berger is wrestling.
“It was fitting to this situation — to attack it head on,” O’Brien said.
The family friend said the 17-year-old is always looking to help out.
“He walks in [the house], and if he sees the garbage is full, he just goes and takes the garbage out,” O’Brien said.
Dinah Berger said her son was in terrible pain one day, and she brought him to Huntington Hospital. Doctors first thought he had kidney stones, but tests found none. A CT scan was ordered after a urine test showed a small amount of blood. When the scan was analyzed, the top part of a tumor could be seen.
An MRI taken at an outpatient facility confirmed the tumor, and the mother took her son to Memorial Sloan Kettering Cancer Center in Manhattan. It was there the family received hope from Berger’s oncologist Dr. Leonard Wexler, even though Dinah Berger said it has been difficult.

Due to Zach Berger’s treatments, the incoming senior will be unable to attend school when it begins in September, according to his mother. In addition to being an honor student, he has been a member of the high school football and wrestling teams. Earlier this year, he placed in the county championships for wrestling.
“We all have our moments, but he’s been trying to be really brave,” Dinah Berger said. “It’s a lot for a 17-year-old to know they’re going to be hit with this.”
His mother, who is divorced from Berger’s father and works part time at two small companies, will take time off from work as her son will need to be taken back and forth to the city for chemotherapy and doctor appointments at MSK. In addition to chemotherapy, his treatment will possibly include surgery and radiation.
“One of the oncologists said this is a full-time job,” she said.
Dinah Berger said there is a possibility that a room will open up at the Ronald McDonald House where they can stay, and eventually the goal is for her son to receive treatment at Sloan’s Commack location.
The mother said the family recently received good news when a PET scan showed that the tumor had not metastasized.
“It’s the happiest news I have had in my life,” she said. “The whole thing is horrible and a nightmare, at least that gave me some hope.”
As of Aug. 1, 205 donations — totaling $16,000 of the $50,000 goal — have been collected. O’Brien said she’s not surprised.
“He’s one of those kids that everyone likes,” she said. “If you were going to support or donate to any family, this would be the family to donate to.”
For more information or to donate, visit www.gofundme.com/f/hsf9ja-zachattack.
Gurwin Healthcare System recognizes honorees at annual Celebration Gala
More than 200 people attended the annual Gurwin Healthcare System Celebration Gala at The Royalton on the Greens in Melville recently, honoring individuals who have made a significant impact in the Gurwin Community.
“We celebrate our community members, staff, board members, and those who have worked tirelessly to spread Gurwin’s mission of providing the highest quality health care services in a warm, loving, secure and dignified environment,” said Stuart B. Almer, President and CEO of Gurwin Healthcare System.
Arthur Katz, Founder of Knockout Pest Control, Inc. was the recipient of the 2023 Corporate Honoree Award. Mr. Katz has been a longtime advocate and supporter of Gurwin since the original nursing home welcomed its first resident in 1988.
In addition, the Joseph Gurwin Award was presented posthumously to five past board members, individuals who exemplify the qualities of leadership, vision, passion, philanthropy, and the ability to inspire others. Harriet Becker, Rosalyn C. Gordon, Alfred W. Levy, Howard L. Phillips and Lawrence J. Simon all were instrumental in building Gurwin’s vision that shaped the organization’s growth over the past 35 years.
“We honor Arthur, Harriet, Roz, Al, Howard and Larry as partners who have helped us succeed along our journey of serving thousands of residents and their families over more than 3 decades,” said Bert Brodsky, Chair of the Board of Directors at Gurwin Healthcare System.
“We are proud to celebrate our achievements as a community, remember the legacies of those who are no longer with us, and look forward to caring for generations well into the future.”
Mather Hospital rated as high performing by U.S News & World Report
Mather Hospital, 75 North Country Road, Port Jefferson was rated as high-performing in four adult specialties and two procedures and conditions by U.S News & World Report’s 2023-2024 Best Hospitals rankings. Mather was rated as high performing in:
- Gastroenterology & GI surgery
- Geriatrics
- Orthopedics
- Pulmonology & Lung Surgery
- Heart Failure
- Kidney Failure
Northwell’s North Shore University Hospital was ranked No. 1 in the state and in the top 20 hospitals in the nation. Two other Northwell hospitals placed in the top 10 in state rankings, and dozens of programs across the health system were highly ranked. Overall, eight Northwell hospitals were ranked among the best in New York. North Shore University Hospital tied for the best hospital in the state. Lenox Hill Hospital in Manhattan was ranked No. 5, and Long Island Jewish Medical Center tied for No. 6.
Now in its 34th year, Best Hospitals evaluates hospitals in more than 30 medical and surgical services, with the objective of providing patients with data-driven decision tools. U.S. News said that to keep pace with consumers’ needs and the ever-evolving landscape of health care, several refinements are reflected in the 2023-2024 Best Hospitals rankings and ratings.
The 2023-2024 rankings highlight 484 Best Regional Hospitals that deliver high-quality treatment across many areas of care. Of those, 22 hospitals are named to a national Honor Roll for demonstrating exceptional breadth of excellence across clinical specialties.
Visit U.S. News’ website for the full Best Hospitals rankings
Medical Compass: Reducing kidney stone risk
Lowering your sodium intake can help
By David Dunaief, M.D.

Although it’s possible to have a kidney stone without symptoms, more often they present with the classic symptoms of blood in the urine and colicky pain. The pain can be intermittent or constant, and it can range from dull to extremely painful, described by some as being worse than giving birth, being shot or being burned. The pain can radiate from the kidneys to the bladder and even to the groin in males, depending on the obstruction (1).
Stones are usually diagnosed through the symptoms and either abdominal x-rays or non-contrast CT scans.
Unfortunately, the first line treatment for passing kidney stones — at least small ones — involves supportive care. This means that patients are given pain medications and plenty of fluids until the stone(s) pass. Usually stones that are smaller than four millimeters pass spontaneously. Stones closest to the opening of the urethra are more likely to pass through on their own (2).
Generally, if you’ve passed a kidney stone, you know it.
In the case of a stone too large to pass naturally, a urologist may use surgery, ultrasound, or a combination of methods to break it into smaller pieces, so you can pass it. Unfortunately, once a patient forms one stone, the possibility of having others increases significantly over time. The good news is that there are several lifestyle changes you can make to reduce your risk.
How much water do you need to drink?
First, it is very important to stay hydrated and drink plenty of fluids, especially if you have a history of stone formation (3). You don’t have to rely on drinking lots of water to accomplish this, though. Increasing your consumption of fruits and vegetables that are moisture-filled can help, as well.
Do supplements play a role in stone formation?
One of the simplest methods is to reduce your intake of calcium supplements, including foods fortified with calcium. There are two types of stones. Calcium oxalate is the dominant one, occurring approximately 80 percent of the time (4). Calcium supplements, therefore, increase the risk of kidney stones.
When physicians started treating women for osteoporosis with calcium supplements, the rate of kidney stones increased by 37 percent (5). According to findings from the Nurses’ Health Study, those who consumed highest amount of supplemental calcium were 20 percent more likely to have kidney stones than those who consumed the lowest amount (6). It did not matter whether study participants were taking calcium citrate or calcium carbonate supplements.
Interestingly, calcium from dietary sources actually has the opposite effect, decreasing risk. In the same study, those participants who consumed the highest amount of dietary calcium had a 35 percent reduction in risk, compared to those who were in the lowest group. Paradoxically, calcium intake shouldn’t be too low, either, since that also increases kidney stone risk. Changing your source of calcium is an important key to preventing kidney stones.
What role does sodium play in stone formation?
Again, in the Nurses’ Health Study, participants who consumed 4.5 grams of sodium per day had a 30 percent higher risk of kidney stones than those who consumed 1.5 grams per day (6). The reason is that increased sodium causes increased urinary excretion of calcium. When there is more calcium going through the kidneys, there is a higher chance of stones.
Does protein play a role in stone formation?
Animal protein may play a role. In a five-year, randomized clinical trial, men who reduced their consumption of animal protein to approximately two ounces per day, as well as lowering their sodium, were 51 percent less likely to experience a kidney stone than those who consumed a low-calcium diet (7). These were men who had histories of stone formation.
The reason animal protein may increase the risk of calcium oxalate stones more than vegetable protein is that animal protein’s higher sulfur content produces more acid. This acid is neutralized by release of calcium from the bone (8). That calcium can then promote kidney stones.
Does blood pressure impact kidney stones?
Some medical conditions may increase the likelihood of stone formation. For example, in a cross-sectional study with Italian men, those with high blood pressure had a two times greater risk of kidney stones than those who had a normal blood pressure (9). Amazingly, it did not matter whether or not the patients were treated for high blood pressure with medications; the risk remained. This is just one more reason to treat the underlying cause of blood pressure, not just the symptoms. The most productive way to avoid the potentially excruciating experience of kidney stones is to make these relatively simple lifestyle changes. The more that you implement, the lower your likelihood of stones.
References:
(1) emedicine January 1, 2008. (2) J Urol. 2006;175(2):575. (3) J Urol. 1996;155(3):839. (4) N Engl J Med. 2004;350(7):684. (5) Kidney Int 2003;63:1817–23. (6) Ann Intern Med. 1997;126(7):497-504. (7) N Engl J Med. 2002 Jan 10;346(2):77-84. (8) J Clin Endocrinol Metab. 1988;66(1):140. (9) BMJ. 1990;300(6734):1234.
Dr. David Dunaief is a speaker, author and local lifestyle medicine physician focusing on the integration of medicine, nutrition, fitness and stress management. For further information, visit www.medicalcompassmd.com or consult your personal physician.
Dr. Israel Brown joins New York Health
New York Health (NY Health) has announced the addition of board-certified obstetrician and gynecologist Israel K.O.B. Brown, DO, FACOOG. He will practice at 518 Hawkins Avenue in Ronkonkoma and 6277 NY-25A in Wading River.
“We are thrilled to have Dr. Brown join NY Health,“ said Dr. Rohit Reejsinghani, FACP, MBA, Executive Director of NY Health.. “Dr. Brown brings 14 years of experience in Women’s Health and will make a great addition to our practice.”
Dr. Brown brings a wealth of expertise and a patient-centered, holistic approach to his practice. His areas of specialization include Polycystic Ovarian Syndrome and Menstrual Disorders, Endometriosis, and Diabetic Complications in pregnancy.
“I am excited to join NY Health and contribute to their vision and mission of providing healthcare to patients regardless of their backgrounds,” said Dr. Brown.
He is a fellow of the American College of Osteopathic Obstetricians and Gynecologists (FACOOG), as well as a member of the American Congress of Obstetricians and a member of Gynecologists (ACOG), the American Osteopathic Association (AOA).
As an Alum of the National Health Service Corp, Dr. Brown worked with the underserved communities of Fresno County, California, as well as in private practice and speaks English, Twi, Akan, and Guan.
To make an appointment with Dr. Brown, call 631-473-7171.
Dr. Sherwin Zargaroff joins New York Health
New York Health (NY Health) has announced the addition of board-certified urologist Sherwin Zargaroff, MD. Dr. Zargaroff will practice at 5316 Nesconset Highway in Port Jefferson Station.
“Dr. Sherwin Zargaroff will make a wonderful addition to our team of urologists at NY Health,” said Dr. Rohit Reejsinghani, FACP, MBA, Executive Director of NY Health. “His dedication to staying abreast of the latest advancements in the field, combined with his compassionate approach, will ensure that our patients receive the highest quality of care.”
Dr. Zargaroff specializes in kidney stones, enlarged prostate, trouble voiding, overactive bladder, urinary tract infections, sexual dysfunction, low testosterone, urological cancer workups, hypogonadism, varicocele repair, and male infertility.
“The field of urology offers a great balance between the surgical and medical management of a patient’s urological issues,” Dr. Zargaroff said. “Urology has always been at the forefront of innovative technology. When coupled with patient-centered care, we can treat the full patient — by developing individualized, comprehensive care plans.”
He has authored in peer-reviewed journals and has been a speaker at urological conferences across the nation. He is a member of the American Urological Association and is fluent in both English and Farsi languages.
To make an appointment with Dr. Zargaroff, call 631-758-7003.
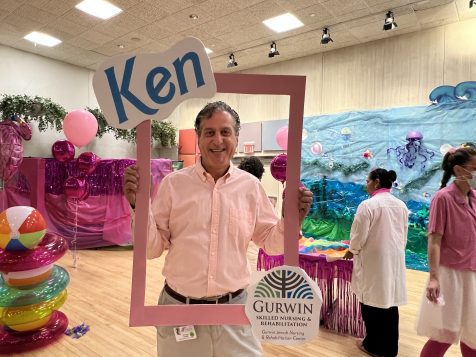
Gurwin Healthcare System hosts Barbie Dream Salon makovers for residents
















Residents and staff of Gurwin Healthcare System in Commack caught “Barbie Fever” days before the release of the new Barbie movie on July 21 with a campus-wide “Barbie-fest” featuring all-pink days of relaxation, fun and resident makeovers at the System’s Gurwin Jewish Nursing & Rehabilitation Center, Gurwin Adult Day Care Program, Gurwin Jewish Fay J. Lindner Residences Assisted Living and Fountaingate Gardens independent living community, on Tuesday, July 18 and Wednesday, July 19.
“Many of our residents remember Barbie’s introduction in the late 1950s and the excitement of getting a brand new doll, or their children grew up with Barbie and they played with the dolls together,” said Nicole Hopper, Director of Therapeutic Recreation at Gurwin Jewish Nursing & Rehabilitation Center. “It really brings back wonderful memories to a simpler time when they could be children themselves.”
The Barbie celebration took place at “Barbie’s Dream Salon,” created by Gurwin staff, dripping in Barbie’s signature Pantone 219 C “Barbie pink” hues. It was there where Gurwin residents had the opportunity to get “Barbiefied,” with manicures, makeup and hot pink hair extensions, all while sipping on Barbie mocktails. Other Barbie-themed activities included paint-your-own Barbie canvas and a Barbie photo booth for social media posting. The celebration extended to Gurwin’s Adult Day Care Programs, where program participants created bedazzled berets for an afternoon “Barbie in Paris” fashion show.
In Gurwin’s senior living communities, staff at Gurwin’s Fay J. Lindner Residences created a Barbie salon and Malibu beach-themed celebration; residents played beach volleyball, posed for Barbie and Ken photos, and created Barbie crafts while enjoying an array of pink-colored delicacies. And, at Fountaingate Gardens independent living community, staff hosted a Barbie pink lemonade and prosecco social with a viewing of the Barbie documentary.
Gurwin staff got in on the BarbieMania, dressing in their best Barbie and Ken-inspired fashions, and posing for photos with residents!
“My daughter had a Barbie collection and it made me feel good when she took care of the dolls as if they were her children,” said Marie Olivia, a 92 year-old-resident of Gurwin Jewish Nursing & Rehabilitation Center. “She had a lot of dolls and we constantly had to wash each of their clothes, press them, then dress them. She was so particular about her dolls that when her friends would come over, they were not allowed to leave until the Barbie’s were put back in their box and safely away.”
“It was truly a remarkable campus-wide celebration for our residents, as well as our staff and visitors,” said Stuart B. Almer, President and CEO of Gurwin Healthcare System. “Our amazing team pulled out all the stops to bring the Barbie pop culture phenomenon event to life at Gurwin for our residents to experience and enjoy.”