Physical inactivity is the greatest risk factor for women over 30
By David Dunaief, M.D.

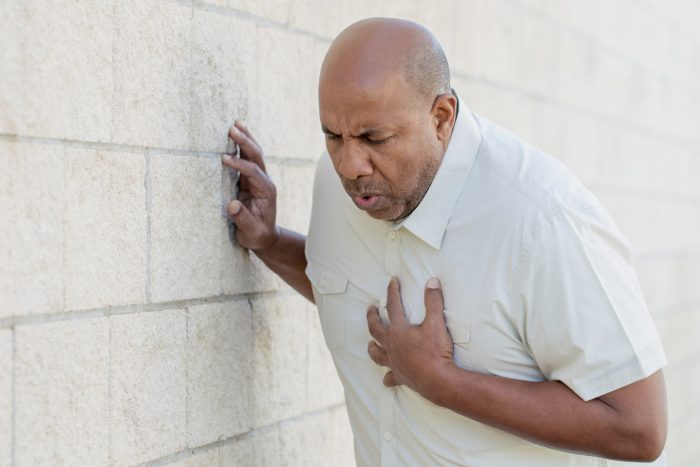
Heart disease is still the number one cause of death in the U.S., responsible for one in five deaths (1).
Many risk factors are obvious, but others are not. Family history, high cholesterol, high blood pressure, obesity, sedentary lifestyle, diabetes and smoking are among the more obvious ones. In addition, age can a role in your risk: men at least 45 years old and women at least 55 years old are at greater risk. Less obvious risks include atrial fibrillation, gout and osteoarthritis.
In practice, we have more control than we think. You can significantly reduce your risk by making some simple lifestyle changes. How much does lifestyle really affect heart disease risk? Here’s one indicator.
In the Nurses’ Health Study, which followed 120,000 women for 20 years, those who routinely exercised, ate a quality diet, did not smoke and were a healthy weight demonstrated a whopping 84 percent reduction in the risk of cardiovascular events, such as heart attacks (2). Inspired? Let’s take a closer look at different factors.
Does your weight really affect your heart disease risk?
Obesity is always a part of the heart disease risk discussion. How important is it, really?
Results from the Copenhagen General Population Study showed an increased heart attack risk in those who were overweight and in those who were obese – with or without metabolic syndrome, which includes a trifecta of high blood pressure, high cholesterol and high sugar levels (3). “Obese” was defined as a body mass index (BMI) over 30 kg/m², while “overweight” included those with a BMI over 25 kg/m².
Heart attack risk increased in direct proportion to weight. heart attack risk increased 26 percent for those who were overweight and 88 percent for those who were obese without metabolic syndrome.
What does this suggest? Obesity, by itself, without blood pressure, cholesterol or sugar level issues, increases your risk. Of course, those with metabolic syndrome and obesity together were at greatest risk, but without these, your risk is still higher if you’re carrying extra pounds.
How important is physical activity to heart disease risk?
Let’s consider another lifestyle factor, activity levels. An observational study found that these had a surprisingly high impact on women’s heart disease risk (4). Of four key factors — weight, blood pressure, smoking and physical inactivity — lack of exercise was the most dominant risk factor for heart disease, including heart attacks, for those over age 30.
For women over age 70, the study found that increasing physical activity may actually have a greater positive impact on heart disease risk than addressing high blood pressure, losing weight, or even quitting smoking. The researchers noted that women should exercise on a regular basis to most significantly reduce their heart disease risk.
What effect does increasing your fiber have?
Studies show that dietary fiber decreases the risks of heart attack and death after a heart attack. In an analysis using data from the Nurses’ Health Study and the Health Professionals Follow-up Study, results showed that higher fiber plays an important role in reducing the risk of death after a heart attack (6).
Those who consumed the most fiber had a 25 percent reduction in post-heart attack mortality when compared to those who consumed the least. Even more impressive is that those who increased their fiber intake after a cardiovascular event experienced a 31 percent mortality risk reduction.
The most intriguing part of the study was the dose response. For every 10-gram increase in fiber consumption, there was a 15 percent reduction in the risk of post-heart attack mortality. For perspective, 10 grams of fiber is just over eight ounces of raspberries or six ounces of cooked black beans or lentils.
You can substantially reduce your risk of heart attacks and even potentially the risk of death after sustaining a heart attack with simple lifestyle modifications. Managing your weight, increasing your physical activity and making some updates to your diet can lead to tremendous improvements.
How long do you suffer with osteoarthritis?
Traditional advice for those who suffer from osteoarthritis is that it is best to live with hip or knee pain as long as possible before having surgery. But when do we cross the line and consider joint replacement?
In a study, those with osteoarthritis of the hip or knee joints that caused difficulty walking on a flat surface were at substantially greater risk of cardiovascular events, including heart attack (5). Those who had surgery for the affected joint saw substantially reduced heart attack risk. If you have osteoarthritis, it is important to improve your mobility, either with surgery or other treatments.
References:
(1) cdc.gov. (2) N Engl J Med. 2000;343(1):16. (3) JAMA Intern Med. 2014;174(1):15-22. (4) Br J Sports Med. 2014, May 8. (5) PLoS ONE. 2014, 9: e91286 (6) BMJ. 2014;348:g2659.
Dr. David Dunaief is a speaker, author and local lifestyle medicine physician focusing on the integration of medicine, nutrition, fitness and stress management. For further information, visit www.medicalcompassmd.com or consult your personal physician.