With 694 more people testing positive for the coronavirus, the number of confirmed cases in Suffolk County is now 40,483.
In the Suffolk County hotspot testing sites, the number of positive tests was 1,320 out of 3,412 total tests.
The percentage of positive tests at these hotspots is 38.7, compared with 33 percent for the county as a whole.
Antibody testing for law enforcement continues, with 1,581 law enforcement officers tested by Northwell Health and New York State so far.
The number of people who have died from complications related to coronavirus increased by 21 in the last day, bringing the total to 1,568 for Suffolk County. As of yesterday, the deaths from the virus exceed the number of people killed over 100 years ago aboard the Titanic. The staggering number represents what will likely be a turning point for the county, let alone the entire country which topped 77,000 deaths.
County Executive Steve Bellone’s (D) office distributed another 163,000 pieces of personal protective equipment yesterday, bringing the total number of such life-saving items to over four million since the crisis began in March.
Bellone didn’t have the closely watched hospitalization information today because the reporting system was down.
Separately, Bellone said the county was able to honor the 75th anniversary of the end of World War II in Europe.
“Today, we would normally be bringing together our veterans and particularly our World War II veterans to honor them and thank them for what they did for our nation,” said Bellone during his daily call with reporters.
A group including Suffolk County Chief of Police Stuart Cameron and Suffolk County Veterans Services Agency Director Thomas Ronayne raised an American flag above Armed Forces Plaza today. The group saluted the flag and then brought it to the state veteran’s home.
That home has been hit especially hard by the pandemic. As of May 5, the home reported 65 residents have passed away due to the coronavirus. Additionally, 68 residents have tested positive, where out of those four are receiving treatment at neighboring Stony Brook University Hospital. 30 of those veterans are in the post-COVID recovery phase.
Bellone said the county also celebrated the graduation of 70 members of the police academy. While the ceremony was different than it otherwise would have been prior to the pandemic, the event, which was broadcast on Facebook, was watched by more than 25,000 people.
“Their willingness to step forward at any given moment to risk their lives for strangers is an extraordinary thing,” Bellone said. “We thanked them and their family members.”
Separately, as for the national and local elections coming this November, Bellone said he hopes the bipartisan cooperation that has characterized the response in Suffolk County and New York will continue.
“I don’t know if we’re going to see that on a national level [but] at the local level, we are working together in ways we haven’t in many years, maybe not since 9/11,” Bellone said. “That’s what we should do.”
Bellone suggested the county didn’t have “time to spare to worry about partisan nonsense.”
He pointed out how he and Comptroller John M. Kennedy Jr. (R), who ran against Bellone to become county executive, have been “working closely together to address issues here. I’m hopeful that will continue.”
Stony Brook Closes Satellite ER
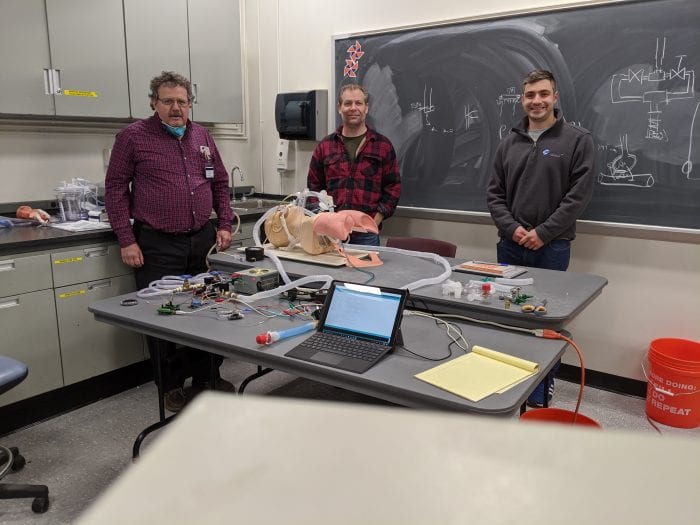
Stony Brook University is closing the emergency room field satellite in the South P Lot amid a decline in the number of patients.
The hospital will keep equipment inside the tents in case of future need. The health care workers who had been staffing the field site will return to the hospital.
Stony Brook had seen approximately 2,600 patients at the coronavirus triage sites.
The drive-through testing site in the South P Lot will remain open. That site has tested 27,515 patients.
Residents who would like a test need to make appointments in advance, by calling 888-364-3065. The site is open seven days a week, 7 a.m. to 7 p.m.
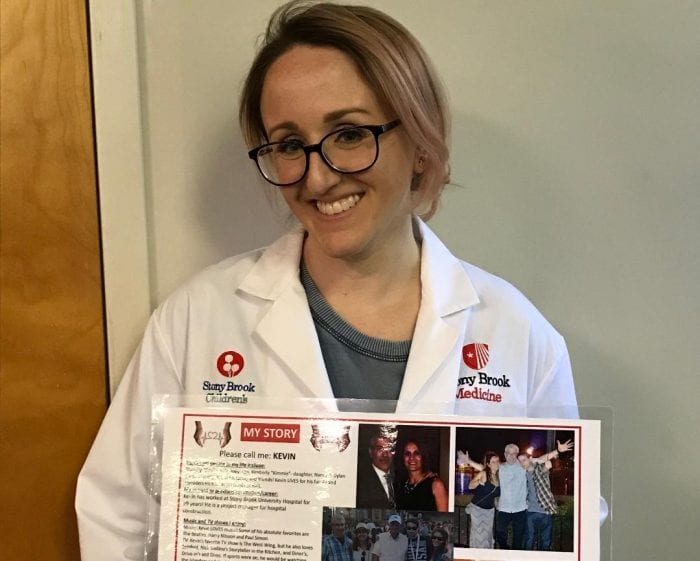
Stony Brook University Hospital’s Team Lavender, and a Staff Support Team, delivered care packages to the employees at the Long Island State Veterans Home. The team put together 170 containers filled with donated items from the community including gum, chapsticks, drinks and snacks. They also included trays of home-baked goods, crocheted ear savers, and masks made by a veteran.
Team Lavender volunteers include doctors, nurses, social workers, patient advocates, chaplains, a faculty and staff care team, employee assistance program and employee health program. The team provides emotional, spiritual and psychological support for faculty and staff after an adverse or unexpected event.