In response to an easing of state regulations and their approach to patient care, area hospitals are relaxing restrictions about patient visitors.

Starting this past Monday, Huntington Hospital will allow patients who do not have COVID-19 to have one visitor per day, between 2 p.m. and 6 p.m. St. Charles and St. Catherine of Siena hospitals also allow one COVID-19 negative visitor per day during those same hours.
Huntington Hospital is responding to the medical, emotional and personal need its patients have for the support of family and friends during whatever health challenges they face.
“There is nothing like having your loved one at your bedside, holding your hand,” said Cheryl Miranda, director of Patient Experience at Huntington Hospital, which is a part of Northwell Health.
Family also provides helpful information, helping medical professionals know whether a patient’s behavior is different from normal
“As a nurse, I’ve always felt that family is part of the caregiving circle,” Miranda said. “The family knows their loved one better than anyone. They will help us provide better care.”
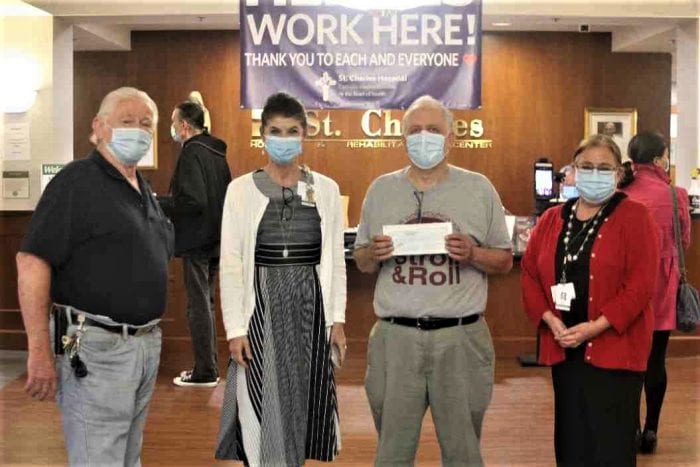
St. Charles Hospital and St. Catherine of Siena started allowing one hospital visitor per COVID-negative patient per day starting about four weeks ago.
Stony Brook is making several changes to its visitation policy.
As of April 1, the hospital is allowing two visitors for patients in labor and delivery, for pediatric patients and for patients in end-of-life situations. This will increase from one to two.
Patients receiving same day surgical procedures will also be allowed a patient visitor until a procedure begins. The visitor is required to wait outside during the procedure and then can return during the patient’s release from the hospital.
Inpatient child psychiatry will also allow a visitor, as will cancer center and outpatient offices.
Approved visitors to Stony Brook must wear a mask that covers their nose and mouth the entire time, will have symptom checks, including thermal scanning, will not be allowed outside the patient’s room, must maintain six feet of distance and must wash their hands on entering and leaving the room.
Hospitals had generally restricted most or all patient visitors over various periods in the last year amid the pandemic to limit the spread of COVID-19. Nurses throughout Long Island and the world have used tablets, phones and other technology to help their patients connect with family members, enabling them to see spouses, siblings, children, grandchildren and friends from hospital beds that often had them feeling isolated during their health battles.
Allowing visitors, who are still required to wear masks, will help hospitalized patients feel more normal and receive the kind of support that can brighten their day while shortening their hospital visit.
A hospital employee will screen patients on their way into the hospital, asking them questions about any possible symptoms and taking their temperature.
Visitors who are COVID-19 positive can’t enter. Additionally, visitors who come in from out of the state or whom they believe necessitates a screening will have a rapid swab.
“We are not asking everyone to be tested,” Miranda said.
The hospital is spreading the word about its new patient visitor policy by changing its on-hold messages, is sharing information on TV sets and is telling families directly during virtual visits that one person at a time can come to the hospital.
Patients can determine who visits, which includes family members and friends.
“There is nothing like having your loved one at your bedside, holding your hand.”
— Cheryl Miranda
Miranda said the medical staff is well-prepared for an increase in visitors through the hospital.
“I don’t have to tell anybody in this building to follow precautions,” Miranda said. “We’ve all been through this for 13 months now and there isn’t anyone” who needs reminding about personal protective equipment, hand washing or social distancing.
Initially, Huntington Hospital workers will escort visitors to patient rooms, reminding them about safety policies.
During visits, patients and visitors are expected to wear masks. If a family member comes during mealtime or brings food, the patient can eat, but should do so at a safe distance.
Miranda, who has been at Huntington Hospital for 20 years, realizes the suffering patients and their families have endured during the pandemic.
“To tell someone they can’t be here is an awful, awful thing,” Miranda said. “My heart goes out to the families that haven’t been allowed to be here” and to the patients who “haven’t been able to have their loved ones at their side.”
Miranda has been planning this new visitation policy since the beginning of the month.
The hospital has learned numerous lessons about health care, including by providing virtual support for patients.
In addition to bereavement support groups, which have been particularly busy as families mark the one-year anniversary of the loss of a loved one, the hospital is adding a long-haul support group.
Starting on Thursday, April 8 at 2 p.m., Huntington Hospital will offer support to people who have a lingering cough, ongoing debilitating fatigue, body aches, joint pain, shortness of breath, loss of taste and smell, difficulty sleeping, headaches and brain fog.
People interested in joining that group can email Kacey Farber at [email protected].
Dr. Jean Cacciabaudo, associate medical director at Huntington Hospital and a cardiologist, will sit on the long haulers support meeting. Cacciabaudo, who had COVID-19 and has some long haulers symptoms, will attend not just for herself, but to provide the physician’s perspective.
Miranda said the bereavement support groups have helped family members amid a loss.
“It’s the beauty of humanity, when we reach out and help each other,” Miranda said. “There’s no magic solution for grief and loss. For some people, it’s just about remembering all the wonderful things they had when they had that person and sharing that with other people. It’s about not being isolated. That’s a big key.”