Northwell Health has announced that after serving as Northwell’s first president and chief executive officer for more than 23 years, Michael J. Dowling will step down effective October 1, 2025 and transition to the role of CEO Emeritus, where he will serve in an advisory capacity, supporting the advancement of key public health initiatives, and focusing on teaching and writing, according to a press release on May 14.
Dowling’s transition marks the end of an extraordinary tenure characterized by significant growth, industry innovation, and a steadfast commitment to enhancing health for all. Over the past two decades, his visionary leadership has transformed Northwell from a network of Long Island-based hospitals into one of the nation’s ten largest health systems, renowned for its clinical, academic, and research excellence. Under his leadership, Northwell became New York State’s first integrated health system in 1992 and now includes 28 hospitals across New York and Connecticut, employing 104,000 individuals, with over 14,000 affiliated physicians, 1,000 care locations, and a comprehensive network of home care, rehabilitation, and end-of-life services.
As president and CEO of Northwell, Michael Dowling spearheaded the system’s remarkable expansion, championing investments in research, leading to the growth of the Feinstein Institutes for Medical Research and positioning Northwell at the forefront of bioelectronic medicine. His dedication to innovative medical education through the Zucker School of Medicine, the Hofstra-Northwell School of Nursing, and Northwell’s Center for Learning and Innovation has cultivated the next generation of health care professionals.
Additionally, Dowling has taken a leadership role in addressing gun violence, the leading cause of death among children in the United States, recognizing it as a critical health care issue. He has mobilized over 60 health care CEOs nationwide to support gun violence prevention. For 18 consecutive years, he has been named to Modern Healthcare magazine’s list of the “100 Most Influential People in Healthcare,” achieving the magazine’s #1 ranking in 2022.
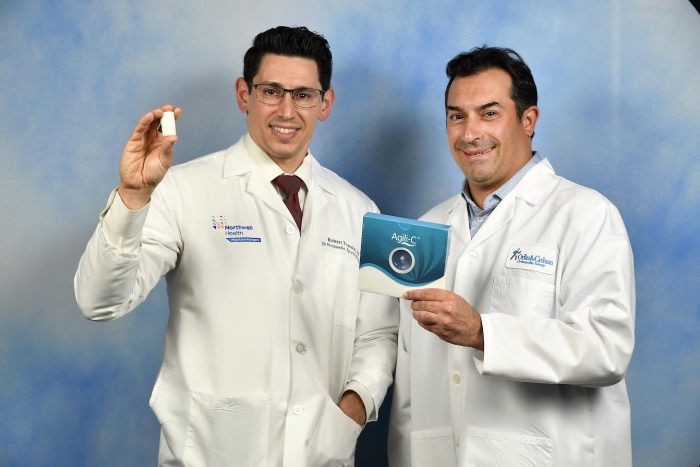
Above, Dr. John D’Angelo will succeed Dowling in the fall.
After an extensive nationwide search, and confirmed in a unanimous vote, Northwell’s Board of Trustees has appointed John D’Angelo, MD, who currently serves as executive vice president of the health system’s central region, to succeed Dowling as president and CEO in October. Dr. D’Angelo began his more than 25-year tenure at Northwell as an emergency medicine physician at Glen Cove Hospital before advancing into health system-wide clinical and administrative leadership roles.
“It has been an extraordinary privilege to lead Northwell through a period of unprecedented growth and clinical transformation that has enabled our team members to make a meaningful difference and improve the lives of the tens of millions of patients and families who we’ve cared for over the last 25 years,” said Dowling in the release.
“In Dr. D’Angelo, the Board of Trustees has selected a tremendous leader who will lead Northwell to greater heights. John is someone who understands and champions Northwell’s unique and differentiated culture and his clinical and operational acumen coupled with skills as a decisive and collaborative leader will enable Northwell to raise the bar on the quality of care we deliver to the communities we serve in New York and Connecticut. I look forward to partnering with Dr. D’Angelo in the coming months to help ensure a seamless transition to what will be an exciting new chapter in the 33-year history of Northwell,” he added.
“I am humbled and honored to be selected to succeed Michael Dowling as Northwell President and CEO. I am committed to build on his unparalleled legacy and vision that grew Northwell from a Long Island-based health system into a regional and national health care leader,” said Dr. D’Angelo. “Health care is a calling. Every minute of every day, we have an opportunity to change someone’s life for the better, and I look forward to leading our more than 100,000 team members who contribute to this critically important mission. Together, we will continue advancing better health for all.”
As president of Northwell’s central region, Dr. D’Angelo leads a dynamic health care network serving 2.8 million residents in western Nassau County and Queens, a network that includes six hospitals, over 270 ambulatory practice locations, and a dedicated team of 24,000 employees. During the COVID-19 pandemic, Dr. D’Angelo was at the forefront, orchestrating Northwell’s operational response and later becoming Chief of Integrated Operations, charged with streamlining system operations in the post-pandemic era.
Before this role, Dr. D’Angelo was the senior vice president of Northwell’s Emergency Medicine service line, where he managed 18 emergency departments and a network of 60+ urgent care centers, serving 1.5 million patients annually. With nearly three decades of experience as an emergency medicine physician, Dr. D’Angelo possesses a deep understanding of clinical care delivery, quality, process improvement, and operational management.
“The Northwell Board of Trustees is enormously grateful for Michael Dowling’s extraordinary tenure, and we are delighted to name Dr. D’Angelo as our next CEO,” said Board Chair Margaret Crotty. “Dr. D’Angelo is an experienced administrator, leading a region that itself would rank among the country’s largest health systems. He is a trusted mentor for so many Northwell leaders; a respected manager who inspires his team to consistently drive results; and a strategic leader who deploys technology toward the best health outcomes. John clearly stood out among an impressive slate as the best person to bring Northwell into a new era of care.”