By Daniel Dunaief
While she hasn’t resolved the debate about two approaches to a type of heart surgery, Laurie Shroyer, Professor and Vice Chair for Research in the Department of Surgery at Stony Brook University’s Renaissance School of Medicine, has contributed considerable information over a long period of time.

In a recent study released in JAMA Surgery, Shroyer, who is the principal investigator and co-PIs Fred Grover and Brack Hattler of the Rocky Mountain Regional Affairs Medical Center, revealed that coronary artery bypass grafting had similar post-surgical death rates for the veterans in their study whether the surgeon used a heart-lung machine, called “on pump,” or performed the surgery without the machine, called “off pump.”
Using long-term results from 2,203 mostly men at 18 VA Centers in the Department of Veterans Affairs Randomized On/Off Bypass (ROOBY) trial, Shroyer determined that the death rate at 10 years was 34.2 percent for off-pump, compared with 31.1 percent for on-pump.
Patients typically need bypass graft surgery when they have a narrowing of their coronary arteries, which comes from fatty material accumulating in the walls of the arteries. Doctors take a part of a healthy blood vessel from the leg, wrist or elsewhere and bypass the blockage, building a detour for the blood and enabling better circulation in the heart.
Using the “off pump” procedure means doctors operate on a heart that’s still pumping blood through the body. The “on pump” procedure uses a heart lung machine to pump blood while the heart remains still.
While the results of this study don’t end the debate over whether one procedure is superior to another, doctors welcomed the data as a well-researched and detailed analysis.
“There’s always going to be this ever-last question of whether off versus on pump bypass surgery is better,” said Dr. Henry Tannous, Chief of Cardiothoracic Surgery at the Renaissance School of Medicine at Stony Brook University. “There’s always going to be very little nuances with different patients that will make us pick one or the other.”
Dr. Tannous who has performed the majority of all bypass surgeries at Stony Brook over the last five years, said the hospital offers surgeries with and without the pump. SB has doctors who specialize in each kind of bypass in case of a change in the expected procedure.
Doctors typically get a clear sense of whether a patient might benefit from on or off pump procedures before starting surgeries. In the great majority of cases, doctors perform the surgery according to their pre-planned expectations for the use of the pump.
Rarely, they convert to the other procedure based on inter operative findings that dictate the switch, Dr. Tannous explained.
Dr. Jorge Balauger, Associate Chief of Cardiothoracic Surgery and Director of Advanced Coronary Surgery, has performed 4,000 CABG procedures, including about 1,000 without the heart lung machine, or “off pump.”
In his considerable experience, he suggested that an 80-year old, who has renal or liver dysfunction and/or arteries in his or her neck that are partially blocked or had another type of comorbidity, such as something in the bone marrow, would not tolerate a heart lung machine well. A person with cirrhosis also would likely be better served with an off pump operation.
“Avoiding the heart lung machine on the older, sick patients is beneficial,” Dr. Balauger said, adding that he looks at the CABG procedure as being akin to a “tailor made suit” that has to fit the patient specifically.
In cases where patients need a second bypass procedure, Dr. Balauger also recommends off pump efforts because a second operation on pump is “way more complex” and requires “dissection of all the scar tissue around the heart, which makes it not only time consuming, but also risky.”
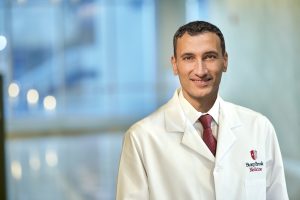
Dr. Tannous appreciates the perspective Shroyer brings to the discussion. “Sometimes, it’s an asset to have a researcher and statistician with a very scientifically oriented mind lead the study,” he said, adding that when surgeons meet with patients, they will discuss the use of the pump.
Dr. Baulager described the trial conducted by Shroyer as having an “excellent design” from a scientific standpoint.
He believed, however, that the study didn’t include surgeons who had sufficient expertise in off pump procedures. Dr. Baulager thought more experienced surgeons likely ensured better outcomes for off pump procedures.
One aspect of the study that was “refreshing” to Shroyer was how durable the surgical procedure is, with about 70 percent of patients who received this procedure, both on and off pump, still experiencing improvements in their pre-surgical chest pain symptoms after 10 years.
“We never expected the high proportion of patients would do so well longer term in terms of freedom from events, and in terms of symptoms,” she said. “The fact that the symptoms weren’t different between on and off pump is good news.”
After this type of study, Shroyer will work with several other trials to identify if certain sub-groups of high risk patients may have benefits from an off pump procedure.
To be sure, Shroyer cautioned that these results couldn’t be extrapolated to the general population, especially to women, as almost all of those the study followed were men.“Veterans are a unique population,” she said. “Many received cigarettes as part of their rations, and hypertension is quite high. They are a different population in terms of their [health care] complexities and their [underlying] illnesses.”
While the 10 year outcomes were similar, Shroyer found a shorter revascularization-free survival period among off pump patients.
Dr. Tannous said this kind of study would generate considerable interest among cardiac surgeons.
“Everything [Shroyer] has written about bypass surgery from the ROOBY trials will catch any cardiac surgeon’s attention nationwide,” he said. “This paper is not any different. It has the extra long-term follow up that makes it more relevant.”