By Daniel Dunaief
Researchers at Brookhaven National Laboratory, Cold Spring Harbor Laboratory and Stony Brook University joined the chorus of moviegoers who enjoyed and appreciated the Universal film Oppenheimer.
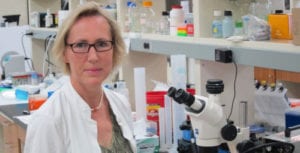
“I thought the movie was excellent,” said Leemor Joshua-Tor, Professor and HHMI Investigator at Cold Spring Harbor Laboratory. “It made me think, which is always a good sign.”
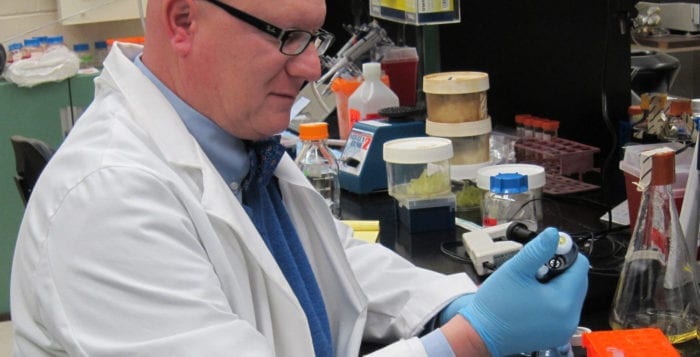
Yusuf Hannun, Vice Dean for Cancer Medicine at Stony Brook University, thought the movie was “terrific” and had anticipated the film would be a “simpler” movie.
Jeff Keister, leader of the Detector and Research Equipment Pool at NSLS-II at Brookhaven National Laboratory, described the movie as “interesting” and “well acted.”
Joshua-Tor indicated she didn’t know anything about Robert Oppenheimer, the title character and leader of the Manhattan Project that built the atomic bomb. She “learned lots of new things” about him, she wrote. “I knew he was targeted by McCarthy-ism, but didn’t realize how that came about and the details.”
Keister also didn’t know much about Oppenheimer, who was played by actor Cillian Murphy in the film. “Oppenheimer seemed to quietly struggle with finding his role in the story of the development of the atomic bomb,” Keister said. “At times, he wore the uniform, then later seemed to express regret.”
Like other researchers, particularly those involved in large projects that bring together people with different skills and from various cultural backgrounds, Oppenheimer led a diverse team of scientists amid the heightened tension of World War II.
Oppenheimer was “shown to have been granted an extremely powerful position and was able to form a relatively diverse team, although he was not able to win over all the brightest minds,” Keister wrote.
Joshua-Tor suggested Oppenheimer “charmed” the other scientists, who were so driven by the science and the goal that they “accepted him. The leader of the team should be a great scientist, but doesn’t necessarily have to be the biggest genius. There is a genius in being able to herd the cats in the right way.”
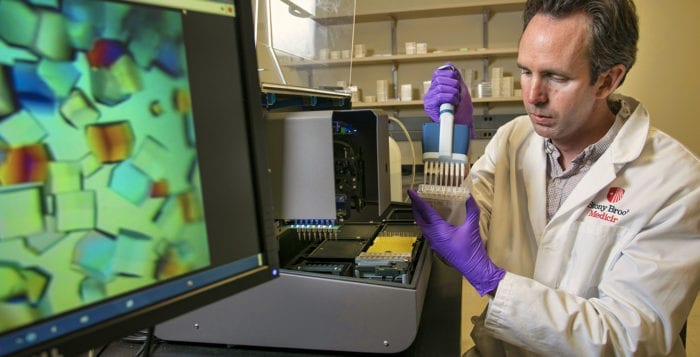
Joel Hurowitz, Associate Professor in the Department of Geosciences at Stony Brook University, “loved” the movie. Hurowitz has worked with large projects with NASA teams as a part of his research effort.
Hurowitz suggested that the work that goes into coordinating these large projects is “huge” and it requires “a well laid out organizational structure, effective leadership, and a team that is happy working hard towards a common goal.”
‘Stunning’ first bomb test
Keister described the first nuclear bomb test as “stunning” in the movie. “I have to wonder how the environmental and health impacts of such a test came to be judged as inconsequential.”
Some local scientists would have appreciated and enjoyed the opportunity to see more of the science that led to the creation of the bomb.
Science is the “only place the movie fell short,” Hannun said. “They could have spent a bit more time to indicate the basic science behind the project and maybe a bit more about the scientific accomplishments of the various participants.”
Given the focus of the movie on Oppenheimer and his leadership and ultimate ambivalence about the creation of the atomic bomb, Keister suggested that scientists “could be better encouraged to understand the impacts of applied uses of new discoveries. Scientists can learn to broaden their view to include means of mitigating potential negative impacts.”
Research sponsors, including taxpayers and their representatives, have an “ethical responsibility to incorporate scientists’ views of the full impacts into their decisions regarding applications and deployment of new technology,” Keister said.
Joshua-Tor thinks there “always has to be an ongoing conversation between scientists and the citizenry” which has to be an “informed, somewhat dispassionate conversation.”
Recommended movies about scientists
Local researchers also shared some of their film recommendations about scientists.
Hurowitz wrote that his favorite these days is Arrival, a science fiction film starring Amy Adams. If Hurowitz is looking for more lighthearted fare, he writes that “you can’t go wrong with Ghostbusters,” although he’s not sure the main characters Egon, Ray and Peter could be called scientists.
Keister also enjoys science fiction, as it “often challenges us with ethical dilemmas which need to be addressed.” While he isn’t sure he has a favorite, he recommended the sci-fi thriller Ex Machina starring Alicia Vikander as a humanoid robot with artificial intelligence,.
Joshua-Tor recalls liking the film A Beautiful Mind starring Russell Crowe and Jennifer Connelly as John and Alicia Nash. She also loved the film Hidden Figures, starring Taraji P Henson, Octavia Spencer and Janelle Monáe.