They lost patients, sleep and time with their families and yet, through some of the most difficult conditions in over a century, they persevered, brought together by the shared goal of saving lives threatened by the pandemic.
The Times Beacon Record Newspapers is pleased to honor the health care workers who put themselves in harm’s way to offer comfort, cures and solutions for COVID-19.
State Sen. Jim Gaughran (D-Northport) described health care workers as “heroes beyond belief.” He added, “There are folks who have gotten sick and died, simply because they were just doing their jobs.”
Unusual Requests
Indeed, in some cases, these health care workers took on tasks that aren’t typically a part of their job description or training.

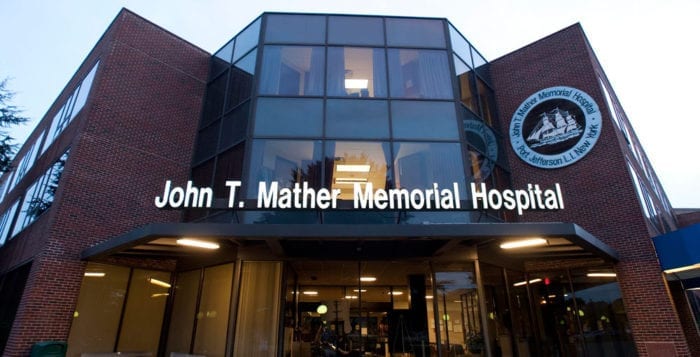
Take Kristen Thomas, a registered nurse at Mather Hospital in Port Jefferson. A priest came up to her in the halls of the hospital to ask for an unusual favor. A person had died and the family, who couldn’t be by his side, asked for last rites. The priest knew he couldn’t enter the room.
He asked, “Would you mind taking holy water and anointing the patient?”
She approached the patient, made the sign of the cross and prayed, as the priest stood outside the door.
“A moment like that, you never really plan to do that,” Thomas said. “We tried to give the family a little bit of closure. They didn’t get to attend the normal [rituals].”
For the community and health care workers, normal took on new meaning, especially in the first few months of the pandemic, when Suffolk County became an epicenter of the virus.
With family unable to sit by the bedside, nurses often stepped up, holding up iPad and phones so the family could spend time together virtually.
Marilin Dilone, Emergency Department nurse at Stony Brook University Hospital, called the young family of one of her patients.

His wife “put the baby on the phone — the baby looked like he was maybe 10 months old. The baby was making noises. I swear [the patient] opened his eyes. The wife is crying. Such a moment, we take for granted. He could hear her say, ‘I love you.’ To be able to provide that was very humbling for me.”
Like Dilone and so many other nurses, Robert Collins, a nurse at Mather Hospital ,shared how he held an iPad up to patients whose conditions were deteriorating so they could say goodbye to their families.
He had to stay in the room because some of the patients couldn’t hold the iPad.
“You do that once or twice, it kind of sticks with you,” Collins said.
Deep Connections
The connections the medical staff made to the families of patients extended well beyond the typical interactions.
“We had patients for an extended period of time,” said Patricia Coffey, nurse manager of the Critical Care Unit at Huntington Hospital.
Coffey, who spent 11 weeks actively caring for patients as her managerial duties “went to the wayside,” said the staff talked to families for extended periods of time. She spoke with some families daily, spending as much as two-and-a-half hours each day on the phone.
The nurses felt like members of the family because the normal support system couldn’t provide bedside support.
“You were channeling the family to the patient,” Coffey said. The nurses were “rooting so hard” for the patients.
When one of those patients who was in the hospital died after a long battle, she said it was “unbelievably heartbreaking — you felt like one of your own family members had died.”
She still keeps in touch with family members.

Coffey said one of her neighbors was admitted to the hospital with COVID and was on her floor. Coffey’s children and her neighbor’s children grew up together and their daughters were friends.
She not only spoke with his wife every day during her 60-hour weeks, but she also called her coworkers over the weekend to ask how he was doing.
The conversations with the neighbor’s wife were “a little hard. I wanted to be honest with her. He was very critical. At the same time, I was trying to be hopeful. It was a hard balance.”
Coffey said he was “one of the lucky ones who survived.”
Dilone of SBUH described how the work was more physically demanding.
She would “try not to ask for people” as she didn’t want to expose others if it wasn’t necessary. “You are taking care of patients more by yourself, turning them and doing chest PT [physiotherapy] — it was physically more demanding,” Dilone said.
Dark Moments
Watching patients who died took its toll, even on people who have been in the medical profession for decades.
MaryJane Finnegan, chief nursing officer at St. Catherine of Siena Medical Center in Smithtown, described the unusually high number of people dying from the virus. The hospital was running out of space for the dead. The morgue was filled and an additional refrigeration truck outside also filled quickly.

“One day, eight people died — usually in a week, you can have eight people die, but not eight in a day,” Finnegan said.
Nikki Fiore-Lopez, chief nursing officer at St. Charles Hospital in Port Jefferson said a nurse was present for the death of her mentor. Watching her die was “one of the darkest moments” for the nurse, Fiore-Lopez said.
Many medical professionals encouraged their patients to fight through the worst of the virus.
Stony Brook’s Dilone stayed with a patient whose blood oxygen level kept dropping. She wouldn’t let him fall asleep because she was worried he’d get intubated. She reminded him of his family and that he needed to help himself.
“I felt like Nurse Ratched,” Dilone said, referring to the dreaded nurse from the movie “One Flew Over the Cuckoo’s Nest.”
Dilone spent hours with this patient. Later, a doctor told her keeping the man awake prevented him from getting intubated.
Unexpected Challenges
With a virus no one had battled before, health care workers had to be flexible, learning about everything from new protocols for admitting patients to the latest and best treatments.

The staff had to confront the “speed with which everything changed,” said Dr. Eric Morley, associate professor and clinical director in the Department of Emergency Medicine at Stony Brook University’s Renaissance School of Medicine. “Every day, there were new protocols, new ways to deal with things.”
Hospitals had to create a forward triage system to deal with the flood of COVID patients amid all the other potential emergencies hospitals routinely have.
These efforts required hundreds of employees to “get on the same people to sort people out,” Morley said. Training staff to manage the flow of patients required constant communication.
Even some of the smaller elements of managing the crisis took Morley’s time, such as getting new traffic signs to direct people to an alternate site.
Hospital managers were continually confronted with numerous unexpected challenges.
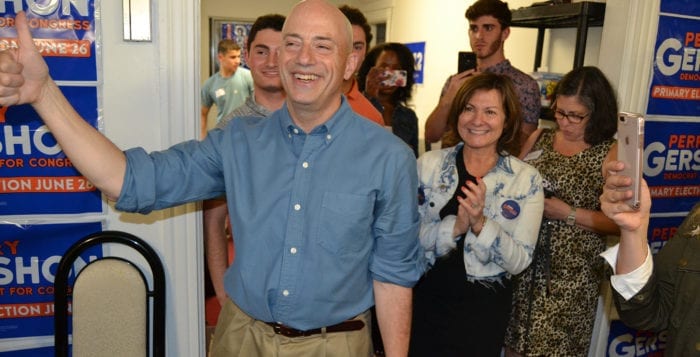
Ken Roberts, president of Mather Hospital, said the hospital had to ensure the PPE was hospital grade and not counterfeit.
“There were a lot of suspicious and unscrupulous suppliers when supply and demand was unbalanced, and everyone was in crisis,” he explained in an email.
Health care workers tapped into their personal skills to connect with patients.
Angel Figueroa, a registered respiratory therapist at SBUH who grew up in New York City and learned Spanish thanks to his Puerto Rican heritage, walked into some rooms and spoke Spanish to patients.
When he greeted patients in Spanish, “I would see their eyes open up [and think], ‘Somebody understands me.’”
They would ask him numerous questions, particularly because the medical information came at them so quickly.
Mather’s Collins described how the routine changed so dramatically the moment he arrived at work.

“Rapid response bells were going off as soon as you walked in,” he said. “You didn’t take your coat off” before patients needed attention. “People were not doing well. That was happening more frequently than before. That was an adjustment.”
On the other side of the struggle, health care workers felt a tremendous sense of relief when patients continued their recoveries at home.
“When people were discharged, the staff was thrilled,” St. Catherine’s Finnegan said. “We’d play the [Beatles] song, ‘Here Comes the Sun.’ A lot of hospitals did that. People would gather as many as possible to wish the person well as they were wheeled out.”
Teamwork
Through the difficulties, though, Morley appreciated the support from the community and the families, along with the teamwork and camaraderie from so many departments and staff that all pulled together.
Roberts expressed similar sentiments.
“I was extremely pleased at the teamwork displayed by all hospital staff during the height of the pandemic,” he said.
The Mather president was also grateful for the letters, cards, donated meals, handmade masks and donated PPE.
“The local communities we serve gave us and continue to give us tremendous support and encouragement,” Roberts said. “That has meant so much to the staff to know that the community was supporting them and recognizing their efforts.”

Coffey, from Huntington Hospital, was impressed with how, even amid such extraordinary and challenging times, numerous groups collaborated.
“In many ways there were positive things — the community, the team, everyone working together,” she said. “Parts of it were so uplifting. As hard and as difficult and sad and heart wrenching [as it was], so many other parts, you just saw such humanity. It was amazing.”
Lasting Thoughts
Finnegan said the staff was incredibly appreciative of all the food local restaurants donated.
In fact, some of them joke that they gained the “COVID-19,” referring to the weight they put on while they were working numerous shifts and benefiting from all the donated food.
Morley “rediscovered” Twinkies during COVID in the break room. He has since been able to lose the weight the snack cakes added.
While gyms were closed, Collins relieved stress by buying a 400-pound tractor-trailer tire that he flipped up and down along his driveway. He also took a sledgehammer and “beat on it.”
The exertion would make him tired enough that the stress would dissipate for the day.

Ultimately, what made an ever-expanding job — that affected so many aspects of health care workers’ personal and professional lives — manageable was the shared sense of purpose and the inspiration people drew from each other.
“The fact that the staff was out there doing it” helped give her energy, St. Charles’ Fiore-Lopez said. “We had patients to care for, we had shifts. We had days and weeks and months to get through. They put one foot in front of the other and I needed to do the same.”
Morley appreciated the way the Stony Brook staff pulled together during an intense and challenging time.
“Although it was grueling, it was a special thing to go through with that group of people,” he said.