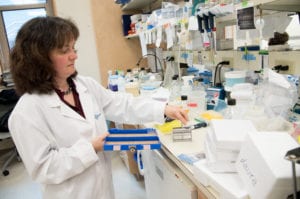
CSHL’s Egeblad shows inflammation activates cancer in mice
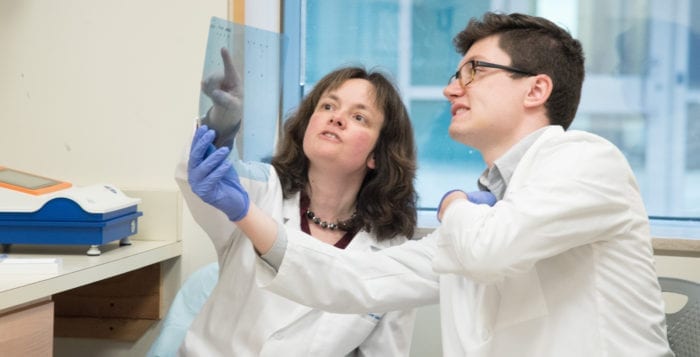
By Daniel Dunaief
For some people, cancer goes into remission and remains inactive. For others, the cancer that’s in remission returns. While doctors can look for risk factors or genetic mutations, they don’t know why a cancer may come back at the individual level.
In a mouse model of breast and prostate cancers, Mikala Egeblad, an associate professor at Cold Spring Harbor Laboratory, has found an important driver of cancer activation and metastasis: inflammation. When mice with cancer also have inflammation, their cancer is likely to become more active. Those who don’t have inflammation, or whose inflammation is treated quickly, can keep the dreaded disease in check. Cancer cells “may be dormant or hibernating and not doing any harm at all,” she said. “We speculated what might be driving them from harmless to overt metastasis.”
Egeblad cautioned that this research, which was recently published in the journal Science, is on mice and that humans may have different processes and mechanisms.
“It is critical to verify whether the process happens in humans,” Egeblad suggested in an email, which she will address in her ongoing research. Still, the results offer a window into the way cancer can become active and then spread from the lungs. She believes this is because the lungs are exposed to so many external stimuli. She is also looking into the relevance for bone, liver and brain metastases. The results of this research have made waves in the scientific community.
“This study is fantastic,” declared Zena Werb, a professor of anatomy and associate director for basic science at the Helen Diller Family Comprehensive Cancer Center at the University of California in San Francisco. “When [Egeblad] first presented it at a meeting six months ago, the audience was agog. It was clearly the best presentation of the meeting!”
Werb, who oversaw Egeblad’s research when Egeblad was a postdoctoral scientist, suggested in an email that this is the first significant mechanism that could explain how cancer cells awaken and will “change the way the field thinks.”
Egeblad credits a team of researchers in her lab for contributing to this effort, including first author Jean Albrengues, who is a postdoctoral fellow. This group showed that there’s a tipping point for mice — mice with inflammation that lasts six days develop metastasis.
Egeblad has been studying a part of the immune system called neutrophil extracellular traps, which trap and kill bacteria and yeast. Egeblad and other researchers have shown that some cancers trick these NETs to aid the cancer in metastasizing.
In the new study, inflammation causes cancer cells that are not aggressive to develop NETs, which leads to metastasis. The traps and enzymes on it “change the scaffold that signals that cancer should divide and proliferate instead of sitting there dormant,” Egeblad said.
To test out her theory about the role of enzymes and the NETs, Egeblad blocked the cascade in six different ways, including obstructing the altered tissue scaffold with antibodies. When mice have the antibody, their ability to activate cancer cells after inflammation is prevented or greatly reduced, she explained.
The numbers from her lab are striking: in 100 mice with inflammation, 94 developed metastatic cancer. When she treated these mice with any of the approaches to block the inflammation pathway, 60 percent of them survived, while the remaining 40 percent had a reduced metastatic cancer burden in the lungs.
If inflammation is a key part of determining the cancer prognosis, it would help cancer patients to know, and potentially treat, inflammation even when they don’t show any clinical signs of such a reaction.
In mice, these NETs spill into the blood. Egeblad is testing whether these altered NETs are also detectable in humans. She could envision this becoming a critical marker for inflammation to track in cancer survivors.
The epidemiological data for humans is not as clear cut as the mouse results in Egeblad’s lab. Some of these epidemiological studies, however, may not have identified the correct factor.
Egeblad thinks she needs to look specifically at NETs and not inflammation in general to find out if these altered structures play a role for humans. “We would like to measure levels of NETs and other inflammatory markers in the blood over time and determine if there is a correlation between high levels and risk of recurrence,” she explained, adding that she is starting a study with the University of Kansas.
Werb suggested that inflammation can be pro-tumor or anti-tumor, possibly in the same individual, which could make the net effect difficult to determine.
“By pulling the different mechanisms apart, highly significant effects may be there,” Werb wrote in an email. Other factors including mutation and chromosomal instability and other aspects of the microenvironment interact with inflammation in a “vicious cycle.”
In humans, inflammation may be a part of the cancer dynamic, which may involve other molecular signals or pathways, Egeblad said.
She has been discussing a collaboration with Cold Spring Harbor Laboratory’s Doug Fearon, whose lab is close to hers.
Fearon has been exploring how T-cells could keep metastasis under control. Combining their approaches, she said, cancer might need a go signal, which could come from inflammation, while it also might need the ability to alter the ability of T-cells from stopping metastasis.
In her ongoing efforts to understand the process of metastasis, Egeblad is also looking at creating an antibody that works in humans and plans to continue to build on these results. “We now have a model for how inflammation might cause cancer recurrence,” she said.
“We are working very actively on multiple different avenues to understand the human implications, and how best to target NETs to prevent cancer metastasis.”