The terror in the opening of the horror movie “When a Stranger Calls” comes when the police tell an anxious babysitter that threatening calls are “coming from inside the house.”
With the killer disease cancer, researchers spend considerable energy and time focusing on signals that might be coming from outside the cell. Many of those signals bind to a receptor in the membrane that corrupt a cell’s normal pathways, leading the cell to uncontrolled growth, the production of tumors or other unhealthy consequences.
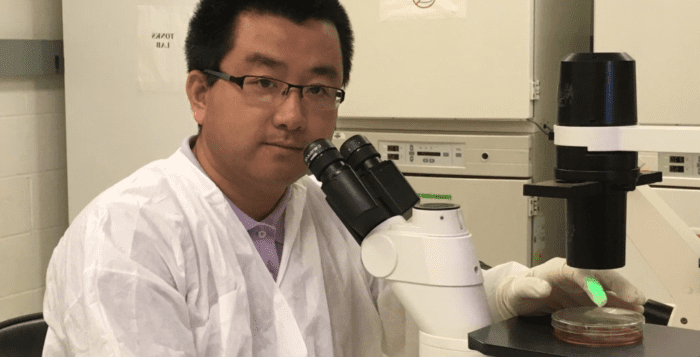
Working in the laboratory of Nicholas Tonks, a professor at Cold Spring Harbor Laboratory, postdoctoral researcher Gaofeng Fan has spent over four and a half years studying a particular signal that comes from inside the cell. I
n a recent study published in Genes & Development, Fan demonstrated that a protein called FER, which adds a phosphate group to the inside part of a receptor called MET, plays a role in the ability of ovarian cancer to spread or metastasize. Already the target of drug development, MET is overexpressed in 60 percent of ovarian tumors. Thus far, developing drugs that block MET alone has not been particularly effective. Indeed, a humanized antibody that prevents human growth factor from binding to this receptor has shown “weak anti-tumor effect” in clinical trials, Fan suggested. In his research in cells, cultures and animal models, Fan demonstrated that ovarian cancer doesn’t spread and may have a different prognosis without FER.
“We found that the ligand [the human growth factor] is not necessary for the activation of the MET,” Fan said. “In the presence of FER, without the ligand, MET can be activated.” Understanding the role of FER in ovarian cancer may offer some clues about why only preventing signals from the outside aren’t enough to protect the cell. While Fan worked with ovarian cancer, he explained other scientists have shown that FER activation has been reported in lung, hepatic, prostate, breast and ovarian cancer. FER plays a part in cell motility and invasion, drug resistance and programmed cell death.
Fan’s work with FER started with a genetic experiment. Taking FER out of a cell, through a process called a loss-of-function assay, Fan found that the cell motility, or its ability to move, decreases. Once he took out FER, he also looked closely at MET activation. If the receptor required only human growth factor, which he included in his experiment, the removal of FER shouldn’t have any effect on its activity. “We found the opposite result,” Fan said.

A set of experiments with mice provided stronger evidence to support his belief that FER played a role in the spread of ovarian cancer. One of the mice had normal FER expression, while the other was missing the FER protein. When he compared the ability of cancer to metastasize, he found that cancer spread in a more limited way in the mice without the protein. “This confirmed the in vitro data and all the cell-based assays,” he said.
After six and a half years as a postdoctoral researcher, Fan is now looking for opportunities to teach and, perhaps, start his own lab in his native China. Fan hopes to continue to work on this system and would like to be a part of the discovery process that might find a small molecule inhibitor for FER. Once he and others find a FER inhibitor, they might be able to use it in combination with other drugs, including small molecules that inhibit human growth factor’s effect on the MET receptor.
Fewer than one in four women with Stage 3 ovarian cancer, which is typically the stage at which doctors find the disease, survive for five years.
Fan said he feels driven to help find a way to slow down the progression of this disease. “There’s an urgency to find a good, effective treatment.” To be sure, Fan cautioned that these studies, while encouraging and an important step in learning about ovarian cancer metastasis, require considerable work to become a part of any new treatment.
In his work, Fan was grateful for the support of Peter A. Greer, a principal investigator at the Cancer Research Institute at Queen’s University at Kingston in Ontario, Canada. Greer “is the leading scientist in research of FER proteins and he opened up all his toolbooks to me,” Fan said.
In an email, Greer described Fan as a “very gifted scientist with an outstanding training experience.” He hopes to “continue our collaboration in the area of ovarian cancer after [Fan] establishes his independent research program” in China. Greer, who spoke with Fan regularly through the process, said he is hopeful that the publication of the study in Genes & Development, in addition to other studies he and other labs have published, will “encourage drug development aimed at FER inhibitors suitable for clinical use.”
Fan also appreciated the guidance and flexibility of his CSHL mentor Nicholas Tonks, famous for his work on tyrosine phosphatase in which he studies the effect of removing phosphate groups. Fan’s research, however, involved understanding adding a phosphate group, through a kinase. “I got humongous support” from Tonks. “Without his help, I couldn’t come this far.”
A resident of Port Jefferson, Fan lives with his wife Yan Xu, who is earning her Ph.D. in materials science at Stony Brook. The couple has a six-year old son, Ruihan, who has enjoyed the Summer Sunday opportunities at Brookhaven National Laboratory, where Ruihan spent hours viewing and constructing the structure of DNA. As for his work, Fan sees opportunities to help people battling this disease.“If we can collect more evidence from this story, we can propose” a way to boost the outcome of treatment, he said.