By David Dunaief, M.D.
NFL players are wearing pink shoes and other sportswear this month, making a fashion statement to highlight Breast Cancer Awareness Month. This awareness is critical since annual invasive breast cancer incidence in the U.S. is 246,000 new cases, with approximately 40,000 patients dying from this disease each year (1). The good news is that from 1997 to 2008 there was a trend toward decreased incidence by 1.8 percent (2).
We can all agree that screening has merit. The commercials during NFL games tout that women in their 30s and early 40s have discovered breast cancer with a mammogram, usually after a lump was detected. Does this mean we should be screening earlier? Screening guidelines are based on the general population that is considered “healthy,” meaning no lumps were found, nor is there a personal or family history of breast cancer.
All guidelines hinge on the belief that mammograms are important, but at what age? Here is where divergence occurs; experts can’t agree on age and frequency. The U.S. Preventive Services Task Force recommends mammograms starting at 50 years old, after which time they should be done every other year (3). The American College of Obstetricians and Gynecologists recommends mammograms start at 40 years old and be done annually (4). Your decision should be based on a discussion with your physician.
The best way to treat breast cancer — and just as important as screening — is prevention, whether it is primary, preventing the disease from occurring, or secondary, preventing recurrence. We are always looking for ways to minimize risk. What are some potential ways of doing this? These may include lifestyle modifications, such as diet, exercise, obesity treatment and normalizing cholesterol levels. Additionally, although results are mixed, it seems that bisphosphonates do not reduce the risk of breast cancer nor its recurrence. Let’s look at the evidence.
Bisphosphonates
Bisphosphonates include Fosamax (alendronate), Zometa (zoledronic acid) and Boniva (ibandronate) used to treat osteoporosis. Do they have a role in breast cancer prevention? It depends on the population, and it depends on study quality.
In a meta-analysis involving two randomized controlled trials, results showed there was no benefit from the use of bisphosphonates in reducing breast cancer risk (5). The population used in this study involved postmenopausal women who had osteoporosis, but who did not have a personal history of breast cancer. In other words, the bisphosphonates were being used for primary prevention.
The study was prompted by previous studies that have shown antitumor effects with this class of drugs. This analysis involved over 14,000 women ranging in age from 55 to 89. The two trials were FIT and HORIZON-PFT, with durations of 3.8 and 2.8 years, respectively. The FIT study involved alendronate and the HORIZON-PFT study involved zoledronic acid, with these drugs compared to placebo. The researchers concluded that the data were not evident for the use of bisphosphonates in primary prevention of invasive breast cancer.
In a previous meta-analysis of two observational studies from the Women’s Health Initiative, results showed that bisphosphonates did indeed reduce the risk of invasive breast cancer in patients by as much as 32 percent (6). These results were statistically significant. However, there was an increase in risk of ductal carcinoma in situ (precancer cases) that was not explainable. These studies included over 150,000 patients with no breast cancer history. The patient type was similar to that used in the more current trial mentioned above. According to the authors, this suggested that bisphosphonates may have an antitumor effect. But not so fast!
The disparity in the above two bisphosphonate studies has to do with trial type. Randomized controlled trials are better designed than observational trials. Therefore, it is more likely that bisphosphonates do not work in reducing breast cancer risk in patients without a history of breast cancer or, in other words, in primary prevention.
In a third study, a meta-analysis (group of 36 post-hoc analyses — after trials were previously concluded) using bisphosphonates, results showed that zoledronic acid significantly reduced mortality risk, by as much as 17 percent, in those patients with early breast cancer (7). This benefit was seen in postmenopausal women but not in premenopausal women. The difference between this study and the previous study was the population. This was a trial for secondary prevention, where patients had a personal history of cancer.
However, in a RCT, the results showed that those with early breast cancer did not benefit overall from zoledronic acid in conjunction with standard treatments for this disease (8). The moral of the story: RCTs are needed to confirm results, and they don’t always coincide with other studies.
Exercise
We know exercise is important in diseases and breast cancer is no exception. In an observational trial, exercise reduced breast cancer risk in postmenopausal women significantly (9). These women exercised moderately; they walked four hours a week. The researchers stressed that it is never too late to exercise, since the effect was seen over four years. If they exercised previously, but not recently, for instance, five to nine years ago, no benefit was seen.
To make matters worse, only about one-third of women get the recommended level of exercise every week: 30 minutes for five days a week. Once diagnosed with breast cancer, women tend to exercise less, not more. The NFL, which does an admirable job of highlighting Breast Cancer Awareness Month, should go a step further and focus on the importance of exercise to prevent breast cancer or its recurrence, much as it has done to help motivate kids to exercise with it Play 60 campaign.
Soy intake
Contrary to popular belief, soy may be beneficial in reducing breast cancer risk. In a meta-analysis (a group of eight observational studies), those who consumed more soy saw a significant reduction in breast cancer compared to those who consumed less (10). There was a dose-response curve among three groups: high intake of >20 mg per day, moderate intake of 10 mg and low intake of <5 mg.
Those in the highest group had a 29 percent reduced risk, and those in the moderate group had a 12 percent reduced risk, when compared to those who consumed the least. Why have we not seen this in U.S. trials? The level of soy used in U.S. trials is a fraction of what is used in Asian trials. The benefit from soy is thought to come from isoflavones, plant-rich nutrients.
Western vs. Mediterranean diets
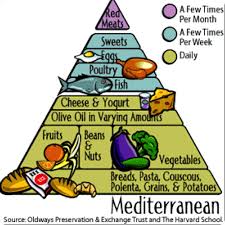
In an observational study, results showed that, while the Western diet increases breast cancer risk by 46 percent, the Spanish Mediterranean diet has the inverse effect, decreasing risk by 44 percent (11). The effect of the Mediterranean diet was even more powerful in triple-negative tumors, which tend to be difficult to treat. The authors concluded that diets rich in fruits, vegetables, beans, nuts and oily fish were potentially beneficial.
Hooray for Breast Cancer Awareness Month stressing the importance of mammographies and breast self-exams. However, we need to give significantly more attention to prevention of breast cancer and its recurrence. Through potentially more soy intake, as well as a Mediterranean diet and modest exercise, we may be able to accelerate the trend toward a lower breast cancer incidence.
References: (1) breastcancer.org. (2) J Natl Cancer Inst. 2011;103:714-736. (3) Ann Intern Med. 2009;151:716-726. (4) Obstet Gynecol. 2011;118:372-382. (5) JAMA Inter Med online. 2014 Aug. 11. (6) J Clin Oncol. 2010;28:3582-3590. (7) 2013 SABCS: Abstract S4-07. (8) Lancet Oncol. 2014;15:997-1006. (9) Cancer Epidemiol Biomarkers Prev online. 2014 Aug. 11. (10) Br J Cancer. 2008;98:9-14. (11) Br J Cancer. 2014;111:1454-1462.
Dr. Dunaief is a speaker, author and local lifestyle medicine physician focusing on the integration of medicine, nutrition, fitness and stress management. For further information, visit www.medicalcompassmd.com or consult your personal physician.