‘Why’ is as important as ‘how’
By David Dunaief, M.D.

Weight loss should be a rather simple concept. It should be solely dependent on energy balance: the energy (kilocalories) we take in minus the energy (kilocalories) we burn should result in weight loss, if we burn more calories than we consume. However, it is much more complicated. Frankly, there are numerous factors that contribute to whether people who want or need to lose weight can.
The factors that contribute to weight loss may depend on stress levels. High stress levels can contribute to metabolic risk factors such as central obesity with the release of cortisol, the stress hormone (1). Therefore, hormones contribute to weight gain.
Another factor in losing weight may have to do with our motivators. We will investigate this further. And we need successful weight management, especially when approximately 70 percent of the American population is overweight or obese and more than one-third is obese (2).

Obesity, in and of itself, was proclaimed a disease by the American Medical Association. Even if you don’t agree with this statement, excess weight has consequences, including chronic diseases such as cardiovascular disease, diabetes, osteoarthritis, autoimmune diseases and a host of others. Weight has an impact on all-cause mortality and longevity.
It is hotly debated as to which approach is best for weight loss. Is it lifestyle change with diet and exercise, medical management with weight loss drugs, surgical procedures or even supplements? The data show that, while medication and surgery may have their places, they are not replacements for lifestyle modifications; these modifications are needed no matter what route is followed.
But the debate continues as to which diet is best. We would hope patients would not only achieve weight loss but also overall health. Let’s look at the evidence.
Low-carbohydrate vs. low-fat diets
Is a low-carbohydrate, high-fat diet a fad? It may depend on diet composition. In the publication of a randomized controlled trial (RCT), the gold standard of studies, results showed that a low-carbohydrate diet was significantly better at reducing weight than low-fat diet, by a mean difference of 3.5 kg lost (7.7 lb), even though calories were similar and exercise did not change (3).
The authors also note that the low-carbohydrate diet reduced cardiovascular disease risk factors in the lipid (cholesterol) profile, such as decreasing triglycerides (mean difference 14.1 mg/dl) and increasing HDL (good cholesterol). Patients lost 1.5 percent more body fat on the low-carbohydrate diet, and there was a significant reduction in an inflammation biomarker, C-reactive protein (CRP). There was also a reduction in the 10-year Framingham risk score. However, there was no change in LDL (bad cholesterol) levels or in truncal obesity in either group.
This study was 12 months in duration with 148 participants, predominantly women with a mean age of 47, none of whom had cardiovascular disease or diabetes, but all of whom were obese or morbidly obese (BMI 30-45 kg/m²). Although there were changes in biomarkers, there was a dearth of cardiovascular disease clinical end points. This begs the question: Does a low-carbohydrate diet really reduce the risk of developing cardiovascular disease (CVD) or its subsequent complications? The authors indicated this was a weakness since it was not investigated.
Digging deeper into the diets used, it’s interesting to note that the low-fat diet was remarkably similar to the standard American diet; it allowed 30 percent fat, only 5 percent less than the 35 percent baseline for the same group. In addition, it replaced the fat with mostly refined carbohydrates, including only 15 to 16 g/day of fiber.
The low-carbohydrate diet participants took in an average of 100 fewer calories per day than participants on the low-fat diet, so it’s no surprise that they lost a few more pounds over a year’s time. Patients in both groups were encouraged to eat mostly unsaturated fats, such as fish, nuts, avocado and olive oil.
As David Katz, M.D., founding director of Yale University’s Prevention Research Center, noted, this study was more of a comparison of low-carbohydrate diet to a high-carbohydrate diet than a comparison of a low-carbohydrate diet to a low-fat diet (4).
Another study actually showed that a Mediterranean diet, higher in fats with nuts or olive oil, when compared to a low-fat diet, showed a significant reduction in cardiovascular events — clinical end points not just biomarkers (5). However, both of these studies suffer from the same deficiency: comparing a low-carbohydrate diet to a low-fat diet that’s not really low fat.
Diet comparisons
Interestingly, in a meta-analysis (a group of 48 RCTs), the results showed that whether a low-carbohydrate diet (including the Atkins diet) or a low-fat diet (including the Ornish plant-based diet) was followed, there was a similar amount of weight loss compared to no intervention at all (6). Both diet types resulted in about 8 kg (17.6 lb) of weight loss at six months versus no change in diet. However, this meta-analysis did not make it clear whether results included body composition changes or weight loss alone.
In an accompanying editorial discussing the above meta-analysis, the author points out that it is unclear whether a low-carbohydrate/high-animal protein diet might result in adverse effects on the kidneys, loss of calcium from the bones, or other potential deleterious health risks. The author goes on to say that, for overall health and longevity and not just weight loss, micronutrients may be the most important factor, which are in nutrient-dense foods.
A Seventh-Day Adventist trial would attest to this emphasis on a micronutrient-rich, plant-based diet with limited animal protein. It resulted in significantly greater longevity compared to a macronutrient-rich animal protein diet (7).
Psyche
Finally, the type of motivator is important, whatever our endeavors. Weight loss goals are no exception. Let me elaborate.
A published study followed West Point cadets from school to many years after graduation and noted who reached their goals (8). The researchers found that internal motivators and instrumental (external) motivators were very important.
The soldiers who had an internal motivator, such as wanting to be a good soldier, were more successful than those who focused on instrumental motivators, such as wanting to become a general. Those who had both internal and instrumental motivators were not as successful as those with internal motivators alone. In other words, having internal motivators led to an instrumental consequence of advancing their careers.
When it comes to health, an instrumental motivator, such weight loss, may be far less effective than focusing on an internal motivator, such as increasing energy or decreasing pain, which ultimately could lead to an instrumental consequence of weight loss.
There is no question that dietary changes are most important to achieving sustained weight loss. However, we need to get our psyches in line for change. Hopefully, when we choose to improve our health, we don’t just focus on weight as a measure of success. Weight loss goals by themselves tend to lead us astray and to disappoint, for they are external motivators. Focus on improving your health by making lifestyle modifications. This tends to result in a successful instrumental consequence.
References: (1) Psychoneuroendocrinol. online 2014 April 12. (2) JAMA 2012;307:491-497. (3) Ann Intern Med. 2014;161(5):309-318. (4) Huffington Post. Sept 2, 2014. (5) N Engl J Med. 2014 Feb 27;370(9):886. (6) JAMA. 2014;312(9):923-933. (7) JAMA Intern Med. 2013;173:1230-1238. (8) Proc Natl Acad Sci U S A. 2014;111(30):10990-10995.
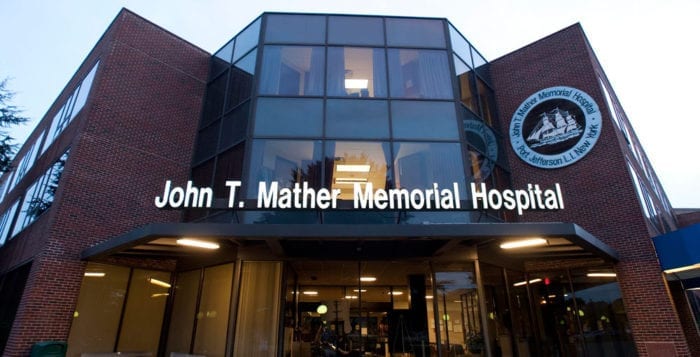
Dr. Dunaief is a speaker, author and local lifestyle medicine physician focusing on the integration of medicine, nutrition, fitness and stress management. For further information, visit www.medicalcompassmd.com.