Her forecast calls for a better summer and a difficult fall and winter.
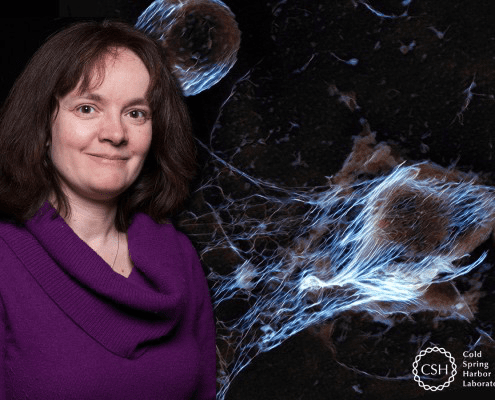
Bettina Fries, the Chief of the Division of Infectious Diseases at Stony Brook Renaissance School of Medicine, sees improvements in the battle against COVID-19 over the next few months, and then a return of stormy weather in the winter.
There will be “much, much less cases in the summer. The reason is that people are more outside and there is less tightness together, but we have to be careful.”
Indeed, a decline in cases of COVID-19 won’t signal a victory over the virus. As the fall approaches, a second wave could exacerbate the typical arrival of the seasonal flu.
“We have a hard winter ahead of us,” Fries acknowledged. As one of several principal investigators involved in efforts to develop an effective treatment for the virus, Fries is working to mitigate the effect of the pandemic.
Fries is overseeing Stony Brook’s involvement in a trial of Regeneron’s drug Sarilumab, which blocks the binding of interleukin-6 to its receptor. The Food and Drug Administration has already approved the drug to treat juvenile rheumatoid arthritis and for the cytokine storm brought on by the treatment of acute leukemia with CAR-T cells.
The work at Stony Brook is a part of Regeneron’s tests in 50 medical centers. At this point, Fries has recruited three of the six patients who will receive the treatment.
Stony Brook is also involved in other studies of potential therapeutics. Sharon Nachman, the chief of the Division of Pediatric Infectious Diseases at Stony Brook Children’s Hospital, has given Remdesivir to two patients with severe symptoms. The drug, which was developed to treat Ebola and Marburg, targets and inhibits the RNA polymerase.
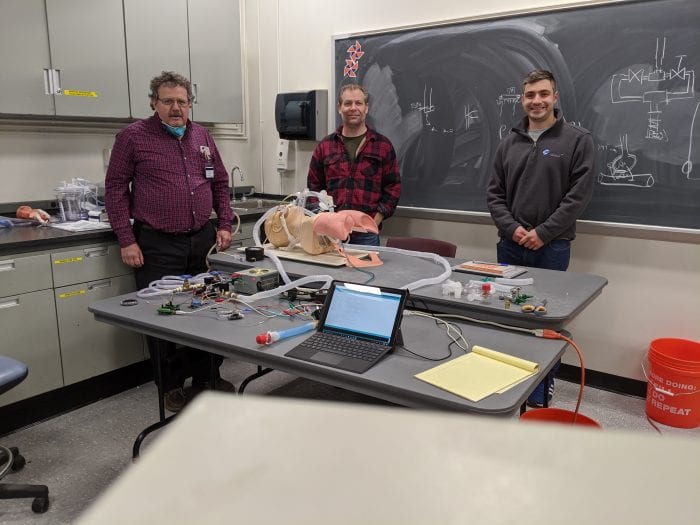
Meanwhile, Elliot Bennet-Guerrero, the Medical Director for Perioperative Quality and Patient Safety for Stony Brook Medicine plans to start a clinical trial of donated, post-convalescent plasma from COVID-19 patients. This approach dates back over 100 years, when serum made from immunized animals helped treat diphtheria.
While each of these approaches could provide relief and extend the lives of people suffering from the virus, Fries doesn’t expect a return to some semblance of normal until the development of a reliable vaccine, which could take another year or more.
Fries sees a potential legal battle developing as countries race to produce a vaccine. She believes the World Health Organization is the group most likely to succeed in ensuring that any effective treatment benefits all of humanity and not just the company or country in which it originated.
“The only organization in my opinion that would be able and have international support to oversee this and make sure this vaccine becomes accessible to everyone and is not getting hung up in patent or licensing disputes is the World Health Organization,” Fries said.
Fries said she believes the international community needs to come to an agreement well before scientists develop an effective vaccine.
“We need everybody in this world to become vaccinated,” Fries said. “It’s really important before we have a vaccine that the international community starts agreeing on what we are going to do if company XYZ in South Korea has the super vaccine first.”
Fries suggested that the American withdrawal from the WHO could prove to be a costly mistake to public health and to global efforts to combat the pandemic.
“Chances are high that the Chinese or Germans or South Koreans will have a vaccine before we do,” Fries said.
As for COVID-19, Fries said the consensus for the infection rate has changed over the last few months, as the virus has spread throughout the world. Indeed, each person who gets the virus now spreads it to about 5.7 other people, which is considerably higher than the rate of between 2.2 and 2.7 researchers had expected from earlier information.
While people who have endured life-threatening symptoms can become infectious, people are generally infectious before they are symptomatic.
As states and countries consider reopening from quarantines, lockdowns and shelter-in-place mandates, Fries said the most effective approach would likely involve a modified reopening with behavioral changes.
Hospitals and urgent care centers can and have changed the way they interact with residents who come into the emergency rooms. The longer-term transition for other businesses and enterprises is more challenging.
Bringing students back to colleges remains a difficult decision that schools around the country face over the next few months, particularly amid a situation in which information about hospitalization, mortality, and testing change by the day.
Sports like swimming and tennis may be able to resume without too many public health alterations, while opera and movie theaters may be more limited in how they can entertain audiences.
Separately, many people have already altered their health care routines, avoiding practices and procedures that could extend the quality and years of their lives. People may not have gotten their chemotherapy and may have missed the chance to get bypass surgery or stents.
“There’s collateral damage we don’t even know yet,” Fries said, “That’s going to be huge.”
Even if the mortality rate is closer to 0.5 percent, the overall number of infections and hospitalizations have “hijacked” the health care system, which can lead to a lower level of care for everyone else, Fries said.
The health care system has been “completely emergency-based for the last 50 days,” Fries observed.
As the country and world approach what might be more of a summer reduction in the numbers, Fries urged ongoing vigilance, even if there are no new cases for an entire month. She suggested that governmental oversight and regulation in connection with a strong health department can help manage through the next wave of cases.
The health care system has had to conquer the seemingly intractable problem of viral deaths, such as from the human immunodeficiency virus, or HIV.
COVID-19 is “very similar in the sense that there was so much despair at the beginning,” Fries said. “When you don’t have a cure, you need to attack a disease with different methods and be okay that you’re not going to cure it, but that you’re going to contain it.”
Fries urged patience as people confront the uncertainty ahead. The ongoing use of masks can help people confront the public health threat that she hopes a vaccine helps conquer.
One of the many clear lessons from this crisis, Fries said, is that those dealing with the public health threat needed to approach it with an understanding of the disruption to the supply chains, with everything from personal protective equipment shortages to ventilators in the right places to adequate staffing of doctors, nurses and other health care professionals.
The garment industry in New York is starting to make plastic coats, Fries said. “Why didn’t we start making that eight weeks ago?”
The same approach also applies to medicines. A multi-disciplinary approach using artificial intelligence could anticipate what hospitals and urgent care centers need, bringing the necessary and vital field of supply chain logistics into this enormous effort.
Ultimately, Fries expects a balance between best practices to keep people safe and the human need for interaction and full engagement professionally and socially.
“We can’t have everybody stay at home,” Fries said. “We have to find a new way of interacting and seeing each other.”
This article was amended April 24 to change the nature in which the drug Remdesivir works.