By Desirée Keegan
Through the efforts of a retired physicist, an orthopedic surgeon from Stony Brook University and a dedicated Haitian who has since moved to Long Island, a 16-year-old from Haiti is on a path with more open doors than ever.
Berlinda was born with two clubbed feet, though she is motivated to better herself, with the dream of one day walking on her own two feet. Steve Kramer, a retired Brookhaven National Lab accelerator physicist met the student in Haiti through Life & Hope Haiti, a nonprofit founded by Haitian-American Lucia Anglade, who built the Eben Ezer School in her hometown of Milot, Haiti.

“She had only been at the school for a few months and she was already learning basic arithmetic,” Kramer said of seeing Berlinda back in March, after meeting her during her introduction to the school in December. “I gave her two columns of work and she handed it back to me with a big smile and said, ‘more.’”
Berlinda has spirit, according to many who have met her, and Kramer was so moved by the story that he reached out to Dr. Wesley Carrion at Stony Brook University School of Medicine’s orthopedics department about performing surgery to fix the girl’s feet. He agreed to do it free of charge.
When he contacted Carrion, Kramer said his secretary Joan mentioned he was deployed in Afghanistan and she didn’t know when he would return. Within a day or two she called to tell him she’d heard from the doctor, who said he’d return by April. In May, the two met.
“I sent him copies of Berlinda’s X-rays and the video and he said he felt he could treat her and rotate the feet, and he would donate his time and get the equipment donated,” Kramer said. “That was a big relief. I felt it might become a reality.”
Carrion had informed Kramer that he would need to get the hospital to donate some of the costs, so Kramer reached out to the Department of Medicine’s Dr. L. Reuven Pasternak, who serves as vice president for health systems and chief executive officer of Stony Brook University Hospital.

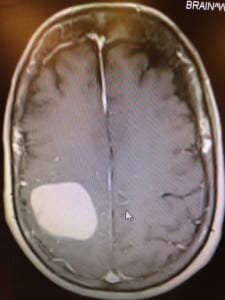
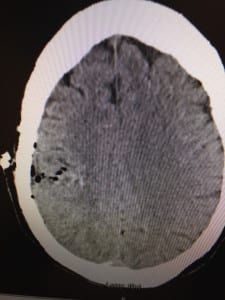
“He said they would cover her hospital costs,” Kramer said after his meeting with Pasternak in July. “This was a bigger relief since beside rotating the club feet we need to check out the status of the hole her spinal column might still have from the spinal bifida she was diagnosed as having. Everyone told me the hole doesn’t close up on its own, but she is doing so well that it may have, but it needs to be checked and closed if it is still open.”
To help bring Berlinda to the United States, Kramer set up a GoFundMe to raise money for her flight cost and other post-operation expenses.
“The fundraising has been going slower than I had hoped, even though everyone I contact is verbally supportive,” he said. “As a physicist my human appeal needs a lot of improvement to really move people to give. But then I look at the video and see the determination she has and feel she will deal with it as she has the tragic events she has already endured and I know she will persevere and will learn to walk.”
Following the surgery, Berlinda will be in the hospital for four months, getting her feet rotated to stretch the tendons as part of the healing process. Her legs will be in cages called external frames that will be attached by pins drilled into her leg bones. Because these create open wounds, it’s best for her to stay the hospital instead of returning to Haiti, to keep the wounds sterile. While recovering, she will continue to go through schooling, which will be one-on-one instead of in a larger classroom back in Haiti.
Without the construction of The Eben Ezer School, Berlinda’s struggles might never have come to light for Kramer. What began as a 10-child school back in 2001 has grown to population over 400, according to Anglade.
“I took the $7,000 I received from my tax return and decided I wanted to build a school in my home country — that had been my motivation,” said Anglade, who now lives in West Babylon. “I’m so blessed. I thank God for that, say thank you all the time. It’s a big school now, and we’re still helping.”

Anglade first visited Berlinda at her house, and heard from the 16-year-old how her brothers and sisters attended school, and she wished she could join them. Because the school is far from her house, she couldn’t walk there.
“I went to her house and she was quiet, said she can’t go to school,” Anglade said. “I told her I was going to help her, and I took her to the school. I pay someone to stay with her at the school. Her dream is to walk, to learn, to be someone. She wants to be happy.”
Kramer and Stony Brook University Hospital are making her dream a reality.
“Thank God for Steve — he has a good heart and I can’t do it by myself,” Anglade said. “With all my heart, I am so happy. Steve has put in a lot of effort to helping Berlinda make her dream come true.”
Kramer first visited the Eben Ezer School through Wading River’s North Shore United Methodist Church in 2015. He joined a group visiting Haiti in February, and has since visited three more times by himself and with Anglade. They are working toward improving the facilities at the school through solar power and updating the water system.
Kramer also provided economic opportunities for students and natives of the town. He cultivated a group of farmers that grow ancient Egyptian wheat, kumat, which is exported to the U.S.
Now, he’s trying to help provide a future for Berlinda.
“She’s very positive, she’s a sponge for learning,” he said. “I just want to help this Haitian girl who has had a tragic life story so far, but has kept her joy of life and has determination to improve herself.”

Amy Miller, of Maine, who has helped Anglade since 2007, said she finds what Kramer is doing admirable.
“I met Berlinda and I really respect his desire to help her move forward,” she said. “You meet someone and they kind of capture your heart, and I think you have to follow your heart. That’s what he’s doing.”
Both said they are also moved by Anglade’s motivation.
“I am tremendously inspired by Lucia,” Miller said. “She’s a force. Lucia is a person that astounds most people that meet her — her energy and her commitment. She loves the kids and it’s wonderful to watch. The community once said she should be their mayor after she brought water to the school she also to the community. She’s quite something.”
Anglade said she’s just doing what she thinks is right, in giving back to her hometown.
“My four kids here go to school, they’re in college, they eat every day, but in Haiti, we don’t have enough to feed over 400 kids, so sometimes when we’re down there for a week or two, we can only feed them for one week,” Anglade said. “I can’t go every week, but if I could go every week, every month, I’d go, just to help them. For me to be able to go down there to help those students, my community, I’m so happy to do it. I really feel good about it.”
To donate to help get Berlinda to the United States and to receive the care and post-treatment she will need, visit www.gofundme.com/BerlindasMiracle. To find out more about Life and Hope Haiti, or to get involved, visit www.lifeandhopehaiti.org.


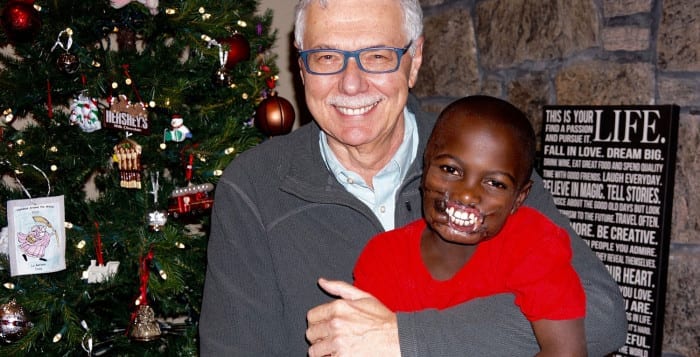



 The surgeries begin in early January, when Dr. Alex Dagum will put three tissue expanders into his face, under the skin on his cheeks and chin. Over a few months, Dagum will slowly fill those with saline, expanding them and stretching the skin. Once there is enough excess skin created, the expanders will come out and that skin will be cut away and used to reconstruct the lips and cheek.
The surgeries begin in early January, when Dr. Alex Dagum will put three tissue expanders into his face, under the skin on his cheeks and chin. Over a few months, Dagum will slowly fill those with saline, expanding them and stretching the skin. Once there is enough excess skin created, the expanders will come out and that skin will be cut away and used to reconstruct the lips and cheek.