Molly came to Stony Brook with an already impressive resume. She is certified by Therapy Dogs International (TDI) and is recognized by the American Kennel Club (AKC) as a Therapy Dog (THD) for her work over the past several years. Besides her visits at Stony Brook University Hospital, Molly is a reading companion for children at a library. Molly is also highly skilled in scent detection. She competes in events that showcase skills similar to bomb or narcotics detection and is currently trialing at the elite level with the National Association of Canine Scent Work (NACSW). Through AKC, Molly earned obedience titles Beginner Novice (BN) and Companion Dog (CD); and has one leg on her Companion Dog Excellent (CDX) title. AKC has also awarded her the Trick Dog Advanced (TDA), Canine Good Citizen (CGC), AKC Temperament Test (ATT) and Farm Dog Certified (FDC) titles.
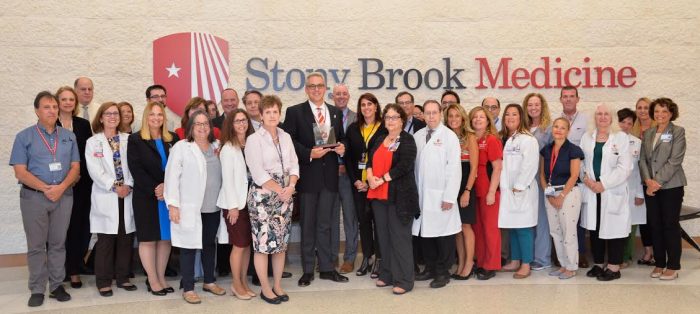
Before the pandemic, Doreen and Molly engaged in hospital visits primarily involving Stony Brook’s geriatric patients. Regular visits were arranged by Carolyn O’Neill, NICHE (Nurses Improving Care for Healthsystem Elders), Elder Life Coordinator and Geriatric Educator at Stony Brook Medicine.
“I have heard countless stories on how visits from Molly and Doreen have greatly benefited our patients,” says O’Neill. “Molly has brought so much cheer to those who need it and she has touched the hearts of many at Stony Brook.” Doreen recalls one patient who had a profound reaction to one of Molly’s visits. After having a stroke, a woman would not talk to anyone. That was until Molly came to see her. After the four-legged volunteer left, the patient’s nurse asked, “What did you think of Molly?” The patient responded, “I love that dog!”

When COVID-19 suspended Volunteer services and in-person visits, Pia York, Therapeutic Intervention Coordinator at Stony Brook Medicine, took the lead to bring virtual Pet Therapy visits to staff. Rounding with an iPad, Pia with help from recreation therapists Chris Brigante, Diane Dignon and Casey Carrick, visited various units bringing tale wags, virtual kisses and tricks to help relieve the stress. They virtually visited every area of the hospital from the pharmacy on the first floor to the 19th floor.
During these visits, Molly became a celebrity. Her name was mentioned hospital-wide and requests for visits increased ten-fold. In addition to visits, Doreen and Molly creatively used photos to help emphasize the importance of social distancing, proper mask wearing, and hand washing to name a few. Some were even written in Spanish. The photos also contained various inspirational messages for Stony Brook staff as they worked tirelessly to care for patients during the height of the pandemic.
Doreen says she simply wants to share the special joy Molly brings. “She always puts a smile on my face and makes me laugh. Patients and staff would often say that Molly made their day,” says Doreen. “When the COVID crisis hit, I thought about the enormous stress and uncertainty at the hospital. Continuing our visits remotely to raise spirits was the least I could do.”
Molly is also a bit of a celebrity outside of Stony Brook. She can be seen running with a little girl at the end of the current Primatene Mist commercial.
To learn more about Pet Therapy at Stony Brook Medicine, visit https://www.