By Daniel Dunaief
An over-the-counter stomach-soothing medication may also relieve some of the symptoms of mild to moderate COVID-19.

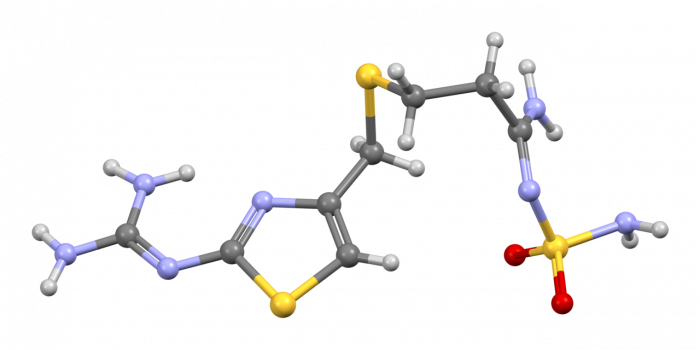
In a study recently published in the journal Gut, Cold Spring Harbor Laboratory Assistant Professor Tobias Janowitz and a team of collaborators at CSHL and The Feinstein Institutes for Medical Research at Northwell Health demonstrated that Famotidine, the active ingredient in Pepcid, shortened the duration of symptoms for a diverse patient group of adults soon after developing COVID-19 symptoms.
In a placebo-controlled study, people taking 80 milligrams of Famotidine three times a day reported that symptoms such as headaches declined after 8.2 days, compared with 11.4 days for patients who were taking the placebo.
“We think that the results are preliminary, but encouraging,” Janowitz explained in an email.
The research, which included 55 volunteers, may offer health care providers another tool to help treat mild to moderate cases of COVID-19. In the clinical study, the use of Famotidine helped reduce a potentially overactive inflammatory response without suppressing the immune system’s efforts to ward off the virus.
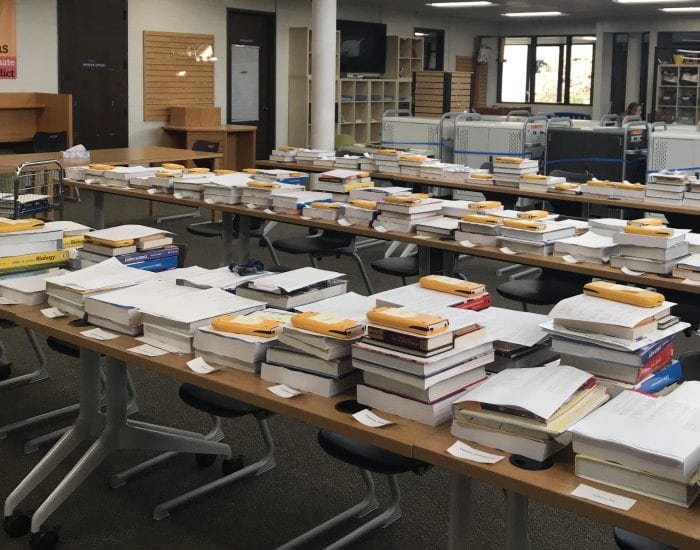
Participants in the study received Famotidine or placebo pills along with a host of instruments they could use at home to gather clinical data about themselves, including a cellular activated Apple iPad, a scale, thermometer, fitness tracker, spirometer to measure air flow in and out of the lungs and a pulse oximeter, which measured oxygen levels by taking a reading over a person’s fingernails.
The protocol for the study allowed volunteers to stay home, where they gathered results from the instruments and reported on their health and any symptoms they felt. Technicians came to the home of each volunteer on the first, seventh, 15th, and 28th days after entering the clinical trial.
Researchers and doctors involved in the analysis of the effectiveness of COVID believe this remote approach to participating in clinical trials could prove a safe and effective way to conduct research for other diseases.
“In today’s virtual world, our clinical trial strategy has significant implications for how to study new drugs in patients at home,” Dr. Kevin Tracey, president and CEO of the Feinstein Institutes, explained in a Cold Spring Harbor Laboratory news brief.
Janowitz added that other studies could also use testing protocols at home, including for other diseases. “We are looking forward to employing it to help develop better treatments for people with cancer,” which is the disease at the center of his research, he explained.
The CSHL Assistant Professor focuses on the whole body response to cancer, although many of the biological considerations are transferable to other diseases.
Pivot to COVID
According to Janowitz, “It was relatively easy for us to pivot to COVID research when it was a global area of unmet need.”
The researchers chose Famotidine because of encouraging studies and from a case series, Janowitz explained. They also found a potential mechanism of action where Famotidine blocked the H2 receptor, which encouraged them to move to a phase 2 randomized clinical trial.
The researchers were pleased that the participants in this small trial included people from a range of ages and ethnic groups. Nearly two thirds of patients, who were 18 years and older, were from black, mixed-race or Hispanic communities.
“Patients with different ancestry may have different responses to this disease,” Janowitz explained. “It helps to learn about the generalizability of the results.”
In a CSHL news brief, Nicole Jordan-Martin, executive director for New York City Health + Hospitals, added that “accessible, safe and low-cost outpatient treatment options are a priority in our global efforts to combat COVID-19.” Northwell and New York City Health + Hospitals provided care for the communities most in need of support for New York City, she added.
The collaborators were also encouraged by their teamwork.
“Our institutions worked extremely well together to face challenges the pandemic posed, like offering digital solutions and reaching populations who struggled for access to care,” Dr. Christina Brennan, vice president of clinical research at the Feinstein Institute and co-investigator of the trial, said in the news brief.
“From screening patients to organizing home delivery of the equipment and medication, this sets a new model for future trials and convenience for participants.”
Janowitz described the safety profile of Famotidine as “excellent” and said it “appears to have few interactions with other drugs and very few side effects in general.”
To be sure, Janowitz cautioned doctors and patients not to stock up on Famotidine before researchers conduct additional studies.
“Our trial is not conclusive and an early phase clinical trial (phase 1 or 2) is not sufficient to inform clinical practice,” he wrote.
Additionally without further study, researchers don’t know the best potential dose and dosing interval for this possible treatment. At this point, they know how long the drug stays in the blood and the strength of its binding to its receptor.
A dose of 20 milligrams per day or less may be too little to achieve an effect, but “we do not know this for certain,” Janowitz explained.
While researchers agreed that further studies were necessary to answer key questions, they believed that the results from this research could provide fodder for studies outside of the COVID world.
“It is possible that sustained inflammation contributes to illness in other contexts and changing this inflammation would be beneficial,” Janowitz wrote. “This will have to be explored separately. Importantly, the methods used in this trial are also transferrable, so we have learned a lot of important information” from this research.