Even as Suffolk County emerges from the worst of the public health crisis from COVID-19, County Executive Steve Bellone (D) expressed concern about the mental health toll the last few weeks has taken on residents.
“Throughout the crisis, we have talked about mental health,” Bellone said on his daily conference call with reporters. “As we move forward, it’s going to become a more important issue.”
People have been reacting to the crisis and helping others. During these stressors, residents have been “going on instinct” and are “exhausted,” Bellone said. “It’s when you start to slow down a bit or move away, that a lot of what you’ve encountered, what you’ve faced can start to manifest itself.”
He anticipates seeing more mental health challenges as the county moves out of this crisis period.
Bellone said he has encouraged residents to contact his office through 311 if they are dealing with mental health challenges, such as depression or anxiety. The Family Service League has provided health care for first responders, health care workers and veterans through a hotline.
The scale of the losses during the pandemic through April has been enormous, Bellone said. With an additional 26 people dying over the last day from complications related to COVID-19, the number of deaths for the county has reached 1,203.
The number of deaths highlights the reason residents in the county need to follow social distancing guidelines and remain at home, to the extent possible. Each day, the county moves closer to the 14-day period during which hospitalizations from COVID-19 decrease, which the county will reach if the declines continue through May 5.
In the last day, 67 fewer people were in the hospital from the virus, bringing the total to 903. Even as some residents were admitted to the hospital, 98 people left the hospital to continue their recoveries at home.
The number of people in the Intensive Care Unit from the virus has also dropped by 20 to 324.
In the last 24 hours, the county has also distributed 37,000 personal protective equipment, bringing the total to over 3.1 million since the pandemic reached Long Island.
Suffolk Forward Business Programs
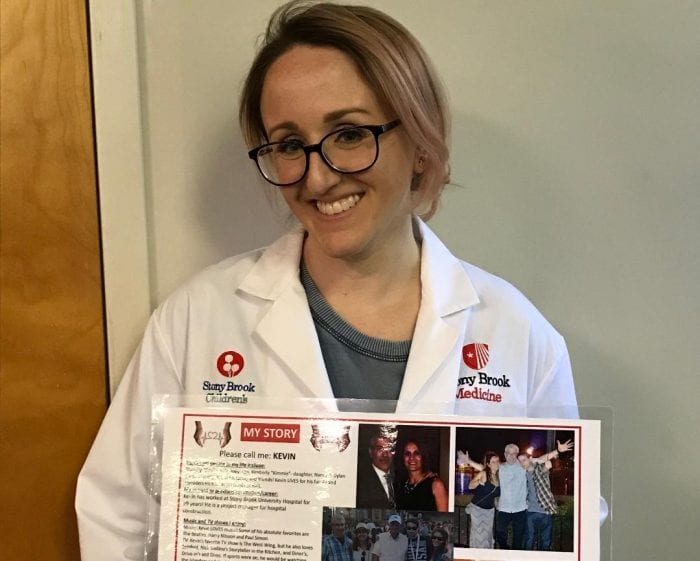
Separately, the county executive announced a program to support small businesses called Suffolk Forward. Designed with Stony Brook University College of Business, the programs were created to help Suffolk County businesses respond to the current economic reality and develop ways to use resources.
Businesses will have the chance to gather information about new ways to increase revenue, build on their technology tools, refine business models, and receive individualized expert business advice.
Suffolk County and its partners will send a needs assessment survey to the restaurant, retail, and construction industries. After reading the replies, Stony Brook University will provide needed services and will report and track the results.
The first effort is the Suffolk Forward Gift Card Platform, which provides a one stop shop for Suffolk County residents to pre-purchase goods and services to support local retail and services businesses during the pandemic. The platform, which was created by Huntington-based eGifter, is free for businesses to participate. To purchase gift cards online, or to have your business feature on the web platform, click here.
The second initiative is the Suffolk Forward Job Board, which provides Suffolk County Residents with access to regional job opportunities and businesses with a pool of applicants seeking new jobs. Suffolk County will provide new details over time.
The last three initiative, Tech Enhancement Program, the Suffolk Forward “Pandemic Shift” Business Workshops, and the Suffolk Forward Virtual Expert Network, provide small businesses with Stony Brook support and education services.
Through the Tech Enhancement Program, local businesses can identify their business technology needs and Stony Brook University business, computer science and IT students, under the direction of faculty, will assess the technology needs of each business and advise the owners. Technology can help businesses reopen during the pandemic and stay open.
The Suffolk Forward “Pandemic Shift” Business Workshops, which are coordinated by the Stony Brook University College of Business, offer a series of four 90-minute video workshops and peer support to help small businesses deal with four key steps: hope, survival, focus and pivot.
The Suffolk Forward Virtual Expert Network provides small businesses with complimentary consultation via virtual office hours with Stony Brook University College of Business professors. The free sessions aim to provide business leaders with the tools that could help them tackle ongoing business challenges.
New York Closes All Schools Until End of School Year
With the question hanging above educators heads for the past month, Gov. Andrew Cuomo (D) finally announced all schools in the state will remain closed until the end of the school year due to the ongoing pandemic. The decision applies to both grade school and higher education, and will mandate the use of distance learning for the next several months.
“Teachers did a phenomenal job stepping up to do this,” Cuomo said. “We made the best of a situation.”
The governor added with the number of school districts and children, it mandates precautions to protect young and old during the pandemic. He said it would not be possible to create a system that would socially distance children while also transporting them and keeping them in schools.
The decision also waives the requirement districts have 180 days of learning per school year.
Regarding in-person summer school, the governor said a decision will be made by the end of May.
On the topic of summer camps, Cuomo said just as he was leaving the press briefing that “whatever regional decision will also apply to the summer camps.”
SC Supervisors Discuss Summer
Meanwhile, the Suffolk County Supervisors Association announced a joint planning effort with three Nassau County Town Supervisors to develop ways to coordinate summer programs across all 13 towns. The group, which Babylon Town Supervisor Rich Schaffer is leading, is known as the Nassau/ Suffolk County Summer Operations Task Force.
The group, which met on Zoom for the first time today, dealt with a number of issues. They wanted to ensure consistent social distancing guidelines across communities.
They also planned to sync the timing of beach, park and facilities as much as they could, to ensure variation among areas doesn’t lead to a surge in crowding at any location. If they needed to close beaches, they also wanted to prevent crowds from forming in any town.
Uniform policies for beach usage, park activity and playground policies will ensure the safest approach to these areas, the supervisors said.
The group announced a goal of May 18 to issue guidelines the towns could agree on.
“Just as we consider the shared service model for other purposes, from purchasing to relieving overcrowding at our animal shelters, inconsistency in policies can lead to greater demand and greater risk at a single location, which we intend to avoid as the purpose of this collaboration,” said Town of Huntington Supervisor Chad Lupinacci (R). “Each Town has something to offer from our parks and beaches to our waterfront facilities — we want our residents and their families to enjoy everything our Towns have to offer without adding unnecessary risk.”
Beaches Open for Hiking and Jogging, not Swimming
Meanwhile, Brookhaven Town will open West Meadow, Cedar in Mount Sinai and Corey in Blue Point.
The Town is not opening the beach at these locations. Prohibited items and activities include chairs, umbrellas, blankets, coolers, fishing, congregating and any sporting activity. Dogs are also not allowed. No lifeguards will be on duty.
Residents will be allowed to walk, hike, and jog at these beaches as long as they maintain social distancing. Masks are recommended. Parking will be limited to 50% of capacity. Code enforcement and parks staff will maintain parking limits and patrol areas to ensure social distancing compliance.
The rules allow for passive uses only. People can’t congregate or engage in sports activities, or use playground equipment. People are also not allowed to shake hands or engage in any unnecessary physical contact. There is no fishing, swimming, blankets, coolers, umbrellas or beach chairs. Social distancing requires six feet between people who don’t live in the same home. When residents can’t social distance, they have to wear face coverings.
Residents with coughs or fever are not permitted. The restrooms are closed. The town encourages people to limit their stays to allow other residents to enjoy the areas. Once the maximum 50% capacity is reached in the parking lots, they will close. As cars leave, others can visit.
With additional reporting by Rita Egan and Kyle Barr