Making sense of loss is never easy, though a Port Jefferson Station family has drawn strength from their 17-year-old son’s bravery and desire to help others, even in his last days.
“Bad things happen to people and this just happened to happen to me, and we’re just going to do the best we can with it,” James Nielsen told his father Steven when they learned the 17-year-old had been diagnosed with a form of cancer so rare and devastating only one documented case of survival exists.

The Comsewogue High School student was diagnosed with NUT midline carcinoma in December 2017, an aggressive form of cancer akin to a death sentence. Despite the devastating prognosis, the Eagle Scout from Troop 454 engaged in rare, barely fleeting moments of despair, according to his parents, even spending the day he died — July 16, 2018 — playing UNO card games and watching the World Cup.
James’ form of cancer is characterized by tumors that form in bones or soft tissue. No effective treatment for NMC exists, there are no guidelines, and current approaches to treatment are based on discussions among a few oncologists who each have had a single experience treating this disease, according to the writings of Dr. Christopher French, a pathologist researching NMC at Dana-Farber/Harvard Cancer Center in Boston, who also advised James’ family after his diagnosis.
“The cancer type that he had is extremely rare and he has a yet even rarer variant of that cancer,” French said in a phone interview. “His tumor was really quite unique. It had a different gene, a variant that is extremely uncommon.”
In late August 2017, upon arriving at cross-country team practice at Comsewogue, James’ mother Jean Nielsen said she noticed a sizable lump on her son’s leg. She said he brushed off her concern, went to practice, and even ran an additional mile when he got home. That night, she had her husband Steven Nielsen examine James’ leg. He said it looked swollen but not necessarily alarming, but when he touched the tumor it was rock solid. A trip that same night to a walk-in medical clinic led to a visit to Stony Brook University Hospital, and by that weekend the family knew their oldest child of four had cancer.
Initially doctors believed he had Ewing’s sarcoma, a diagnosis with a far higher survival rate and clearer treatment options than NMC. In the early stages of his battle, James’ mother said she wrote “treatable and curable” on the first page of a journal the family kept pertaining to his illness. James began what was expected to be a 10-week cycle of chemotherapy, but by the second week of October 2017, it became clear the tumor wasn’t responding to treatment, and immediate surgery would be necessary.
At about 10 p.m. Oct. 12, 2017, just six hours before he was scheduled to head to Manhattan for surgery at Memorial Sloan Kettering Cancer Center, James’ surgeon called and informed his parents there was a possibility he would need to remove their son’s entire leg, and not just portions of the thigh muscle and femur as initially expected.
“I’ll never forget, he looked at us, he sat silent for a moment, and he goes, ‘OK — we’ll do what we have to do,’” James’ father recalled. “And then it was pretty much, ‘Good night.’”
During hour 17 of a 20-hour surgery, the Nielsens were finally informed James would be able to keep his leg.
A positive outlook is often cited as essential in situations like James’, and for the Nielsens positivity flowed on a two-way street.

“I guess we’ve always just kind of been in the place like, ‘It doesn’t help’ — letting your head spin and certainly getting overwhelmed by emotion — you have to kind of keep everything together for him,” Steven Nielsen said. “He made us so strong. We made him strong, but he led the way.”
Being able to salvage his leg was a small, yet short-lived victory. By December, doctors were finally able to pinpoint his diagnosis. Staring down a cancer with such long odds of survival precipitated an unusual response from the Nielsens — a trip to Disney World.
“We didn’t let it control us, we controlled it,” the father said. Self-pity was never in James’ vernacular. “We were never naive about the possibilities of what could happen, but we also, all of us, really felt that it wasn’t worth putting your energy there. Put energy toward your cure. And so we lived life that way.”
The family dedicated their son’s last months to embracing life, spending Thanksgiving evening perusing Manhattan after an eight-hour round of chemo, looking at stores on Madison Avenue, a night his father remembered as “magical.” They visited a ranch in upstate New York just weeks before his death, one of James’ favorite places to vacation. They went to the beach.
While their focus was getting the most of their time remaining, James’ parents were far from ready to give up the fight. Feeling like their experience at Memorial Sloan Kettering left something to be desired, Steven Nielsen did some research that led him to French. James participated in some clinical trials and spent time at the Boston facility, where he and his father even managed to find time to explore the city and visit colleges with notable pharmacy programs, a field in which James had expressed a future interest.
The father’s dogged pursuit of answers for his son led French to mistakenly call him “doctor” during one of their numerous correspondence.
“He wrote in a way that made me think that he knew quite a bit about medicine, I just assumed he was a physician,” French said, laughing. Both Nielsens are teachers in the Comsewogue district.
French is hoping to soon be provided with donated tissue from James for the purpose of research, one of the teen’s dying wishes. His will be the first cancer cell line, which are living cancer cells used for research, with NMC that French will have been able to get his hands on, an essential gift if there’s any hope for untangling the mysteries of the cancer form.
“The tissue that he donated at his autopsy for research was priceless, and potentially a very valuable tool to perform research with,” French said. “He was just a sweet individual. It tore my heart out when I met him very briefly … It was quite riveting to meet him just sort of knowing the truth, that this was likely to not go well.”
For James the decision to donate tissue for research was reflexive and required about two minutes of thought, according to his parents. The teen was known for reusing Dixie cups and napkins because of his aversion to creating waste.

“For him it was just what you do — he didn’t think it was a big deal,” his mother said. “What we look to as heroic or whatever is not really that heroic. Sometimes unassuming people are the most heroic, not people who are very vociferous.”
She said the family can take some comfort in knowing there’s a possibility James’ struggles could lead to a better future for someone else.
“I think if you believe everyone has a purpose, you’d like to think such a horrible result would end with something purposeful, like contributing toward the cure for other people,” the father said. “For us to have him taken away, you hope that that’s the reason.”
The Nielsens expressed gratitude for the support and well wishes they’ve received from the community. Some of James’ classmates have taken up fundraising efforts to get a memorial built in downtown Port Jefferson. Members of the school’s marching band wore pins honoring their fallen peer at the homecoming football game this month. Still, his parents stressed James was not interested in pity or ritualistic gestures of remembrance.
“He was very kind, very sweet, very familial — old kind of qualities that aren’t maybe appreciated as much these days,” his mom said when asked how she hoped he’d be remembered. “He was very selfless.”
To donate to aid in NMC research visit https://www.myjimmyfundpage.org/give/nmcregistryfund.










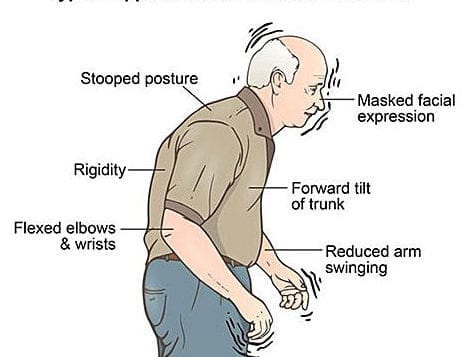
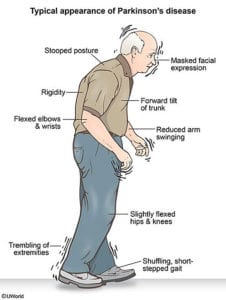 When we typically think of using CoQ10, a coenzyme found in over-the-counter supplements, it is to compensate for depletion from statin drugs or due to heart failure. Doses range from 100 to 300 mg. However, there is evidence that CoQ10 may be beneficial in Parkinson’s at much higher doses.
When we typically think of using CoQ10, a coenzyme found in over-the-counter supplements, it is to compensate for depletion from statin drugs or due to heart failure. Doses range from 100 to 300 mg. However, there is evidence that CoQ10 may be beneficial in Parkinson’s at much higher doses.