To honor his close friend’s fight for life, a Fort Salonga resident took his mark in Staten Island Sunday morning for the run of his.
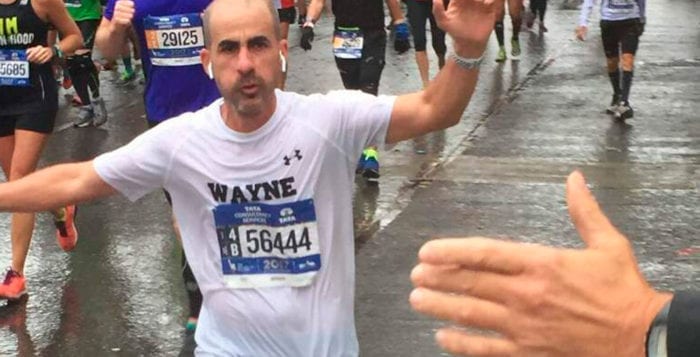
Wayne Trumbull was among the 50,000 participants in the TCS New York City Marathon Nov. 5, running the 26.2-mile race from Staten Island to Central Park to commemorate his friend Paul Gugliuzzo’s perseverance during a harrowing battle with lung failure last year. It was his first time running a marathon.
Trumbull, 50, ran as a member of the American Lung Association team and raised $11,000 for the organization leading up to the marathon. The funds raised will go toward research, advocacy and medical equipment for lung diseases.
Trumbull, a professional tax partner and part-time sports coach, completed the five-borough race with an unofficial time of four hours, 29 minutes, to the roar of thousands of people lining the streets. The loudest of cheers for him came from members of the Fort Salonga community, including Gugliuzzo, who gave Trumbull a high five as he passed by.
“It’s not easy for a casual runner like me to run 26 miles, but when the chips are down, I’m focusing on what Paul went through,” Trumbull said prior to the race. “He was on the brink of death and he bounced back. This is very motivating and emotional for me.”

Gugliuzzo — a Fort Salonga resident, former construction manager and a friend of Trumbull’s since their sons joined the same Kings Park youth baseball team 10 years ago — was diagnosed with upper lobe emphysema and chronic obstructive pulmonary disease in 2009.
His conditions progressively worsened, and in March 2016 he underwent a bilateral lung volume reduction surgery at Columbia Presbyterian Hospital in New York City. His doctors initially advised it would keep him in the hospital for a week. Medical complications occurred, however, and the day after the surgery, Gugliuzzo went into respiratory failure. He was placed into a medically induced coma for five weeks. He spent 107 days in the surgical intensive care unit — during which time his blood was oxidized with an ECMO machine and he battled multiple bouts with pneumonia. He was released from the hospital in August 2016.
Throughout the lengthy ordeal, Trumbull spent every Friday night at his friend’s bedside offering Gugliuzzo’s wife, Patti, and family members a much-needed reprieve as they were there 24 hours a day, seven days a week.
“Wayne supported us at a time when we needed it most,” Patti Gugliuzzo said. “Truly, if it weren’t for Wayne and our friends in Fort Salonga who rallied around us, I don’t know how we would’ve made it.”
It was during these nights Trumbull realized he had to do something significant for Gugliuzzo.
“At that point I didn’t know if it was going to be to honor his life or his battle — fortunately it ended up being his battle,” Trumbull said.
A casual runner who had previously only competed in Northport’s Great Cow Harbor 10K and other smaller races for charity, Trumbull began the process of fundraising for the American Lung Association. He learned that it was a sponsor for the New York City Marathon.
“The marathon was never something I had on my bucket list, but I knew it was significant and something that took a lot of effort and commitment, and would be a fight in and of itself,” he said. “This is just what I consider being a good friend.”
As the 2016 American Lung Association’s team filled its limited spots by the time Trumbull pursued entry, he applied for this year’s team as soon as they took applications. He was part of a strict training program beginning this past summer and ran five days a week for four months in preparation.
Gugliuzzo, who said his lungs are better now than they’ve been in 15 years, is in the process of rehabilitating himself. He’s looking to Trumbull’s participation in the marathon as motivation to hop on the treadmill every once in awhile.
“If Wayne can do 26 miles, I can do two,” Gugliuzzo said. “Me inspiring him in turn inspires me back. It’s heartwarming what he’s done for me.”
He said his hope one day is to run in the Great Cow Harbor 10K alongside Trumbull.












 We know exercise is important in diseases and breast cancer is no exception. In an observational trial, exercise reduced breast cancer risk in postmenopausal women significantly (9). These women exercised moderately; they walked four hours a week. The researchers stressed that it is never too late to exercise, since the effect was seen over four years. If they exercised previously, but not recently, for instance, five to nine years ago, no benefit was seen.
We know exercise is important in diseases and breast cancer is no exception. In an observational trial, exercise reduced breast cancer risk in postmenopausal women significantly (9). These women exercised moderately; they walked four hours a week. The researchers stressed that it is never too late to exercise, since the effect was seen over four years. If they exercised previously, but not recently, for instance, five to nine years ago, no benefit was seen.





























