By Daniel Dunaief
Bringing together researchers and clinicians from six countries, including scientists scattered throughout the United States, a team of scientists co-led by Stony Brook University’s Michael Frohman linked mutations in a gene to congenital heart disease.
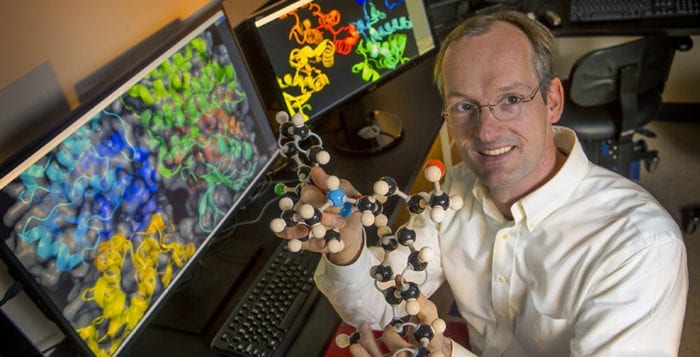
Frohman, Chair of the Department of Pharmacological Sciences in the Renaissance School of Medicine at SBU, has worked with the gene Phospholipidase D1 (or PLD1), for over 25 years. Researchers including Najim Lahrouchi and Connie Bezzina at the University of Amsterdam Heart Center linked this gene to congenital heart disease.
“The current study represents a seminal finding in that we provide a robust link between recessive genetic variants of PLD1 and a rather specific severe congenital heart defect comprising right-side valvular abnormalities,” Bezzina wrote in an email.

The international group collected information from 30 patients in 21 unrelated families and recently published their research in the Journal of Clinical Investigation.
A number of other genes are also involved in congenital heart disease, which is the most common type of birth defect. People with congenital heart disease have a range of symptoms, from those who can be treated with medication and/or surgery for pre-term infants to those who can’t survive.
The discovery of this genetic link and congenital heart disease suggests that PLD1 “needs to be screened in cases with this specific presentation as it has implications for reproductive counseling in affected families,” Bezzina explained.
Bezzina wrote that she had identified the first family with this genetic defect about five years ago.
“We had a strong suspicion that we had found the causal gene, but we needed confirmation and for that, we needed to identify additional families,” she said. “That took some time.
Bezzina described the collaboration with Frohman as “critical,” as she and Lahrouchi had been struggling to set up the PLD1 enzymatic assay in their lab, without any success. Lahrouchi identified Frohman as a leading expert in the study of PLD1 and the team reached out to him.
His work was instrumental in determining the effect of the mutations on the enzymatic activity of PLD1, Bezzina explained.
The timing in connecting with Frohman proved fortuitous, as Frohman had been collaborating with Michael Airola, Assistant Professor in the Department of Biochemistry & Cell Biology at Stony Brook University, on the structure of the PLD1 catalytic domain.
“Together, they immediately saw that the mutations found in the patients were located primarily in regions of the protein that are important for catalysis and this provided detailed insight into why the mutations caused the PLD1 enzyme to become non-functional,” Bezzina wrote.
These findings have implications for reproductive counseling, the scientists suggested.
A couple with an affected child who has a recessive variation of PLD1 could alert parents to the potential risk of having another child with a similar defect.
One of the variants the scientific team identified occurs in about two percent of Ashkenazi Jews, which means that 1 in 2,500 couples will have two carriers and a quarter of their conceptions will be homozygous recessive, which virtually guarantees congenital heart disease. This, however, is about three times less frequent than Tay-Sachs. “This has, in our view, clinical implications for assessing the risk of congenital heart defects among individuals of this ancestry,” said Bezzina.
The mutation probably arose among Ashkenazi Jews around 600 to 800 years ago. There are about 20 known disease mutations like Tay-Sachs in this population that are found only rarely in other groups.
Lahrouchi and Bezzina specialize in the genetics of congenital heart disease, which occurs worldwide in 7 out of every 1,000 live births.
With 56 coauthors, Frohman said this publication had the largest number of collaborators he’s ever had in a career that includes about 200 papers. While this is unusual for him, it’s not uncommon among papers in clinical research.
The lead researchers believed a comprehensive report with a uniform presentation of clinical data and biochemical analysis would provide a better resource for the field, so they brought together research from The Netherlands, the Czech Republic, Israel, France, Italy and the United States.
Previous research that involved Frohman revealed other patterns connected to the PLD1 gene.
About a dozen years ago, Frohman helped discover that mice lacking the PLD1 gene, or that were inhibited by a drug that blocked its function, had platelets that are less easily activated, which meant they were less able to form large blood clots.
These mice had better outcomes with strokes, heart attacks and pulmonary embolisms.
The small molecule inhibitor was protective for these conditions before strokes, but only provided a small amount of protection afterwards. Technical reasons made it difficult to use this inhibitor in clinical trials.
The primary work in Frohman’s lab explores the link between PLD1 and cancer. He has shown that loss of PLD1 decreases breast cancer tumor growth and metastasis.
As for what’s next, Frohman said he has a scientific focus and a translational direction. On the scientific front, he would like to know why the gene is required for heart development. He is launching into a set of experiments in which he can detect what might go wrong in animal models early in the development of the heart.
Clinically, he hopes to explore how one bad copy of the PLD1 gene combines with other genes that might contribute to cause enough difficulties to challenge the survival of a developing heart.
A resident of Old Field, Frohman lives with his wife Stella Tsirka, who is in the pharmacology department and is Vice Dean for Faculty Affairs in the Renaissance School of Medicine. The couple has two children, Dafni, who is a first-year medical student at Stony Brook and Evan, who is a lawyer clerking with a judge in Philadelphia.
Outside of work, Frohman, who earned MD and PhD degrees, enjoys hikes in parks, kayaking and biking.
Having a medical background helped him learn a “little bit about everything,” which gave him the opportunity to prepare for anything new, which included the medical implications of mutations in the PLD1 gene.
Bezzina hopes to continue to work with Frohman, on questions including how the mutation type affects disease severity. “An interplay with other predisposing genetic factors is very interesting to explore as that could also help us in dissecting the disease mechanism further,” she wrote.