By Daniel Dunaief
What if an enormous collection of Scrabble letters were spread out across the floor? What if several letters came together to form the word “victory”? Would that mean something? On its own, the word might be encouraging, depending on the context.
Genetic researchers are constantly looking at letters for the nucleotides adenine, guanine, cytosine and tyrosine, searching for combinations that might lead to health problems or, eventually, diseases like cancer.
For many of these diseases, seeing the equivalent of words like “cancer,” “victory” and “predisposition” are helpful, but they are missing a key element: context.
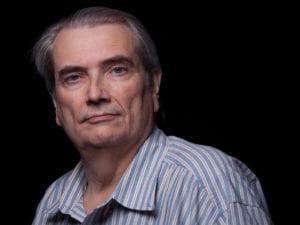
Michael Schatz, an adjunct associate professor at Cold Spring Harbor Laboratory who is also the Bloomberg distinguished associate professor at Johns Hopkins, and W. Richard McCombie, a professor at Cold Spring Harbor Laboratory, use long-read sequencing technology developed by Pacific Biosciences to find genetic variants that short-read sequencing missed.
The two scientists recently teamed up to publish their work on the cover of the August issue of the journal Genome Research. They provided a highly detailed map of the structural variations in the genes of a breast cancer cell.
“This is one of many covers [of scientific journals] that we are pleased and proud of,” said Jonas Korlach, the chief scientific officer at Menlo Park, California-based Pacific Biosciences.
“This is another example of how long-read sequencing can give you a more complete picture of the genome and allow researchers to get a more complete understanding of the underlying biology and here, specifically, that underlies the transition from a health to a cancer disease state,” he said.
Schatz and McCombie were able to see fine detail and the context for those specific sequences. They were able to see about 20,000 structural variations in the cancer genome. “It’s like using Google maps,” explained Schatz in a recent interview. “You can see the overall picture of the country and then you can see roads and zoom out.”
In the context of their genetics work, this means they could see large and small changes in the genome. Only about a quarter of the variants they found could be detected without long-read technology.
In breast cancer, scientists currently know about a family of genes that could be involved in the disease. At this point, however, they may be unaware of other variants that are in those genes. Schatz is hoping to develop more sensitive diagnostics to identify more women at risk.
People like actress and advocate Angelina Jolie have used their genetic screens to make informed decisions about their health care even before signs of any problems arise. Jolie had a double mastectomy after she learned she had the mutation in the BRCA1 gene that put her at an 87 percent risk of developing breast cancer.
By studying the sequence of genes involved in breast cancer, researchers may be able to identify other people that are “at high risk based on their genetics,” Schatz said.
Knowing what’s in your genome can help people decide on potentially prophylactic treatments.
When people discover that they have breast cancer, they typically choose a specific type of treatment, depending on the subtype of cancer.
“There’s a lot of interest to divide [the genetic subtypes] down into even finer detail,” said Schatz, adding, “There’s also interest in transferring those categories into other types of cancer, to give [patients] better treatments if and when the disease occurs.”
The reduced cost of sequencing has made these kinds of studies more feasible. In 2012, this study of the breast cancer genome would have cost about $100,000. To do this kind of research today costs closer to $10,000 and there’s even newer sequencing technology that promises to be even less expensive, he said.
Pacific Biosciences continues to see a reduction in the cost of its technology. The company plans to introduce a new chip next year that has an eightfold higher capacity, Korlach said.
Schatz said the long-term goal is to apply this technique to thousands of patients, which could help detect and understand genetic patterns. He and McCombie are following up on this research by looking at patients at Northwell Health.
In this work, Schatz’s group wrote software that helped decipher the code and the context for the genetic sequence.
“The instrument doesn’t know anything about genes or cancer,” he said. “It produces raw data. We write software that can take those sequences and compare them to the genome and look for patterns to evaluate what this raw data tells us.”
Schatz described McCombie, with whom he speaks every day or so, as his “perfect complement.” He suggested that McCombie was one of the world’s leaders on the experimental side, adding, “There’s a lot of artwork that goes into running the instruments. My lab doesn’t have that, but his lab does.”
Working with his team at CSHL and Johns Hopkins has presented Schatz with numerous opportunities for growth and advancement.
“Cold Spring Harbor is an internationally recognized institute for basic science, while Johns Hopkins is also an internationally recognized research hospital and university,” he explained. He’s living in the “best of both worlds,” which allows him to “tap into amazing people and resources and capacities.”
Korlach has known Schatz for at least a decade. He said he’s been “really impressed with his approach,” and that Schatz is “highly regarded by his peers and in the community.”
Schatz is also a “terrific mentor” who has helped guide the development of the careers of several of his former students, Korlach said.
Down the road, Schatz also hopes to explore the genetic signature that might lead to specific changes in a cancer, transforming it from an organ-specific disease into a metastatic condition.
















