By Daniel Dunaief
It’s like a top scorer for another team that the greatest minds can’t seem to stop. Whatever they throw at it, it seems to slip by, collecting the kinds of points that can eventually lead to a life-threatening loss. The scorer is a transcription factor called MYB, and the points it collects can, and often do, lead to breast and colon cancer and leukemia.
Researchers have known for over 30 years that stopping MYB could help with cancer treatment. Unlike other possible targets, however, MYB didn’t seem to have the kind of structural weakness that pharmaceutical companies seek, where developing a small molecule could prevent the cancer signals MYB delivered. Some researchers have decided that drugs won’t stop this high-profile cancer target.
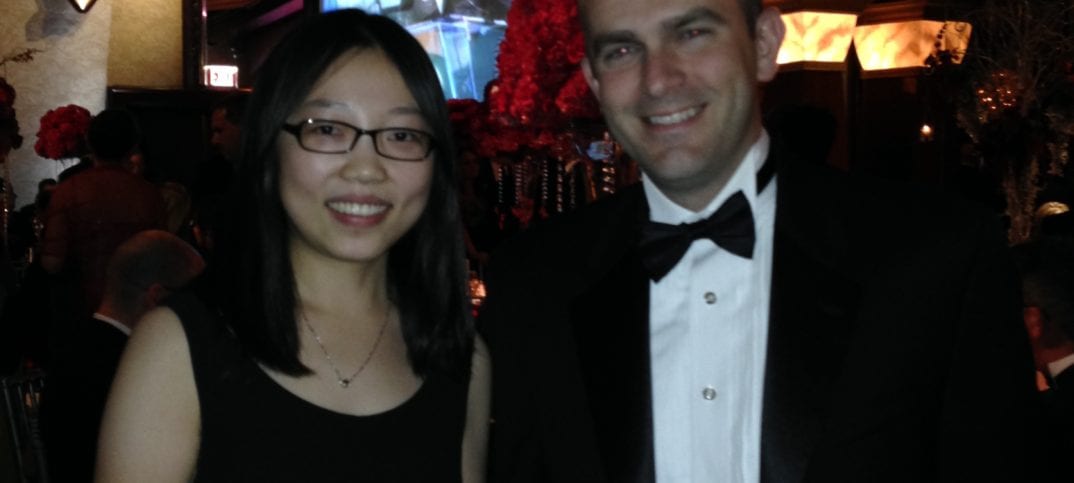
Cold Spring Harbor Laboratory Associate Professor Christopher Vakoc and his graduate research assistant Yali Xu, however, have figured out a way around this seemingly intractable problem. The CSHL scientists recently published their results in the journal Cancer Cell.
MYB binds at a small nub to a large and important coactivation protein called TFIID (which is pronounced TF-two-D). This protein is involved in numerous life functions and, without it, organisms couldn’t survive. Vakoc and Xu found that they could use a small peptide decoy to trick MYB into believing it had attached to this protein when, it reality, it hit the equivalent of a molecular dead end.
In a mouse model of acute myeloid leukemia, this peptide caused leukemias to shrink in size by about 80 percent. “What we’ve discovered is head and shoulders above anything we’ve come across before,” Vakoc said.
As with many scientific discoveries, researchers have to clear numerous hurdles between this conceptual discovery and any potential new cancer therapy. “This is not a medicine a person can take,” Vakoc said.
Indeed, scientists and pharmaceutical companies would need to study what leukemia cells escaped this type of treatment to understand how a cancer might rebound or become resistant after an initial treatment. “Our goal is to develop something with longer lasting effects” that doesn’t become ineffective after three to six months, Vakov said. He described understanding the way a disease reacts to a treatment as an “arms race.” Nature inevitably “finds a way to outsmart our decoy. We’d like to know how [it] does it. We’re always trying to study both sides and trying to anticipate” the next steps.
Down the road, Vakoc could foresee researchers and, ultimately, physicians using this kind of approach in combination with other drugs or therapies, the way doctors now provide patients who have the HIV infection with a cocktail of drugs. Conceptually, however, Vakoc is thrilled that this work “highlights what’s possible.”
One of the most encouraging elements of this approach, Vakoc said, is that it combats MYB without harming organ systems. When the researchers gave the treatment to rodents, the mice were “running around, eating and gaining weight.” Their body tissues appeared normal, and they didn’t demonstrate the same sensitivity that is a common byproduct of chemotherapy treatment, such as losing any hair or having problems in their gut.
An important step in this study, Vakoc said, was to understand the basics of how MYB and TFIID found each other. That, Xu said, was one of the first steps in her graduate work, which took about five years to complete.
In Vakoc’s lab, which includes 13 other researchers, he described how scientists make thousands of perturbations to cancer and normal cells, while they are hunting for cancer-specific targets. By using this screening technique, Vakoc and his team can stress test how cancer cells and normal cells react when they are deprived of certain proteins or genes.
“This began as a screen,” he said. “We took leukemia and normal blood cells and did a precise comparison of the perturbation.” They searched for what had the most specific toxicity and, to their surprise, found that interfering with the binding between MYB and TFIID had the strongest effect. “Once we understood what this nub was doing, we applied all kinds of biochemical assay experiments,” Vakov added.
Ultimately, the peptide they found was a fragment of a larger protein that’s active in the cell. Vakoc credits Xu for her consistent and hard work. “When we started on this hunt, we had no idea where this was headed,” he said. Xu was “relentless” in trying to find the answers. “She pieced it all together. It took a great amount of imagination and intellect to solve this puzzle.”
Vakoc suggested that Xu, who plans to defend her thesis this spring and graduate this summer, has set a great example for the other members of his lab. “I now have 13 other people inspired to outdo her work,” he said. “We know we have a new standard.”
Xu is grateful for the support she has received from Vakoc and appreciates the journey from her arrival as a graduate student from China to the verge of her graduation. “It’s very satisfying when you look back and think how things evolved from the beginning to the end” of her graduate work, said Xu, who lives near Huntington Village and enjoys the chance to visit local restaurants and sample coffee and ice cream when she isn’t conducting research toward her doctorate.
The scientific effort, which was published recently, has attracted the attention of others, particularly those who are studying MYB. Vakoc recently received an email from members of a foundation that is funding research on a solid tumor in which scientists believe MYB plays a role. He is writing grants to get more financial support to pursue this concept. Vakoc is encouraged by the opportunity to make progress with a protein that has been “staring [scientists] in the face for three decades.”