Learn to be…tobacco-free. St. Charles Hospital’s Wisdom Conference Center, 200 Belle Terre Road, Port Jefferson will host a free 7-class tobacco cessation program on Jan. 9, 16, 23, 30, Feb. 6, Feb. 13 and Feb. 27 from 6 p.m. to 7:30 p.m. Make your New Year’s resolution now! For more information or to register, please call 631-853-2928 or 631-853-3162.
New York Cancer & Blood Specialists appoints Rob Negri Chief of Pharmacy
New York Cancer & Blood Specialists (NYCBS) has announced the appointment of Rob Negri as Chief of Pharmacy. In his new role, Negri will continue to lead the pharmacy operations across NYCBS dispensing sites throughout Long Island, New York City, and Hudson Valley, overseeing the team of pharmacists, pharmacy technicians, and oncology nursing staff.
“Rob Negri is a visionary healthcare leader with extensive expertise in pharmacy operations,” said Dr. Jeff Vacirca, CEO of NYCBS. “His leadership will drive New York Cancer & Blood Specialists to further elevate its world-class pharmacy practices, integrating advanced automation and innovative technology to enhance patient care and services.
Negri has previously worked as a Certified Pharmacy Technician for the last 15 years. Prior to joining NYCBS in 2015, Negri worked closely with physicians and pharmacists who provided care at a home infusion pharmacy.
“I am honored to lead an exceptional team of dedicated individuals committed to delivering outstanding care to our patients at NYCBS while ensuring affordable access to essential medications,” said Negri.
For more information, please visit nycancer.com.
Northwell Health’s Michael Dowling recognized as one of Modern Healthcare’s 100 Most Influential People
For the 18th year, the president and CEO of New York’s largest health system has been named to the prestigious list – this year ranking number 35.
Northwell Health has announced that Michael Dowling, president and CEO, was recognized by Modern Healthcare as one of the 100 Most Influential People in Healthcare of 2024, coming in at number 35. The complete ranking can be found in the December issue of Modern Healthcare magazine.
This prestigious recognition program acknowledges and honors individuals who are deemed by their peers and the senior editors of Modern Healthcare to be the most influential figures in the industry in terms of leadership and impact. Michael has consistently ranked among the top leaders in health care on the annual list and was named the most influential in 2022.
“It is an incredible honor to be recognized by Modern Healthcare among such distinguished leaders. This recognition reflects the dedication of the entire Northwell Health team to not only providing exceptional care today, but also building the future of healthcare,” said Mr. Dowling. “At Northwell, we are committed to addressing critical issues like health equity, healthy aging, and gun violence prevention, ensuring that everyone can live a healthier life. Together, we can truly improve the health of everyone in our communities.”
As president and CEO of Northwell Health, he leads a clinical, academic and research enterprise with a workforce of more than 87,000. Northwell is the largest healthcare provider and private employer in New York State, caring for more than two million people annually through a vast network of more than 900 outpatient facilities and 21 hospitals. Under his leadership, Northwell’s annual operating budget has increased to more than $18 billion.
Mr. Dowling is focused on creating the health system of the future. This includes addressing today’s public health infrastructure and the inequities, like addressing Black maternal health disparities, that exist in access to care, especially in underserved communities and communities of color.
He has championed diversity, equity, and inclusion initiatives, resulting in a 90 percent employee satisfaction rate among diverse populations, significantly above the national average. Furthermore, Mr. Dowling has demonstrated a commitment to workforce development through the establishment of the Northwell School of Health Sciencesand a partnership with New York City public schools to create a dedicated health sciences high school.
Since 2019, he has remained a staunch advocate on national issues, including gun violence prevention. Under his leadership, he created the Center for Gun Violence Prevention, has hosted multiple Gun Violence Prevention Forums and has started a wide-reaching public campaign to raise awareness of gun violence. Through the Northwell-initiated National Health Care CEO Council on Gun Violence Prevention & Safety, 54 leading health care CEOs have pledged to leverage their collective influence and resources to curb the historic spike in gun-related deaths and injuries – including a commitment to help fund a $40 million national Ad Council PSA campaign.
Recognizing the inadequacy of most healthcare systems to address the growing needs of an aging population, Mr. Dowling continues to advocate for embracing innovation, technology, and new care models to ensure seniors age with dignity and access the support they need to thrive and to develop solutions to create more age-friendly health systems and improve overall care for our aging population. Just this year, Mr. Dowling coauthored the book, The Aging Revolution: The History of Geriatric Health Care and What Really Matters to Older Adults.
Medical Compass: Eat your way to better cardiac health
Legumes can reduce your risk significantly
By David Dunaief, M.D.

How would you like to be “heart attack proof?” This term was introduced by Dr. Sanjay Gupta and later gained traction when it was iterated by Dr. Dean Ornish. While it’s probably not possible to be completely heart attack proof, research shows us that it is possible to significantly reduce your risk by important lifestyle choices.
About five percent of U.S. adults over age 19 have coronary artery disease (CAD), the most common type of heart disease (1). This contributes to a heart attack rate of one every 40 seconds. We can do better.
Many of the biggest contributors to heart disease risk are well-known: high blood pressure, high cholesterol, and smoking. In addition, if you have diabetes or are overweight or obese, your risk increases significantly. Lifestyle factors, such as poor diet, lack of physical activity and high alcohol consumption are among the significant risk contributors.
This is where we can dramatically reduce the occurrence of CAD. Evidence continues to highlight that lifestyle changes, including diet, are the most critical factors in preventing heart disease. Dietary changes that have a significant impact include consuming dietary fiber, legumes, nuts, omega-3 polyunsaturated fatty acids (PUFAs), and chocolate.
Increase your dietary fiber
We can significantly reduce our heart disease risk if we increase our fiber consumption to recommended levels.
The more fiber you eat, the greater you reduce your risk. In a meta-analysis of 10 studies that included over 90,000 men and 200,000 women, results showed that for every 10-gram increase in fiber, participants experienced a corresponding 14 percent reduction in their risk of a cardiovascular event and a 27 percent reduction in their risk of heart disease mortality (2).
According to a 2021 analysis of National Health and Nutrition Examination Survey (NHANES) data from 2013 to 2018, only 5 percent of men and 9 percent of women get the recommended daily amount of fiber (3). The average American consumes about 16 grams per day of fiber (4).
The Academy of Nutrition and Dietetics recommends 14 grams of fiber for every 1,000 calories consumed, or roughly 25 grams for women and 38 grams for men (5).
Good sources of fiber are fruits and vegetables eaten with edible skin or peel, beans, lentils, and whole grains.

Eat your legumes
In a prospective (forward-looking) cohort study, legumes reduced the risk of coronary heart disease by 22 percent (6). Those who consumed four or more servings a week saw this effect when compared to those who consumed less than one serving a week. The legumes used in this study included beans, peas and peanuts. There were over 9,500 men and women involved, and the study spanned 19 years of follow-up.
I recommend that patients consume a minimum of one to two servings a day, significantly more than the relatively modest four servings a week used to achieve statistical significance in this study.
Include healthy nuts
Why should you include nuts? In a study with over 45,000 men, consuming omega-3 polyunsaturated fatty acids (PUFAs) led to significant reductions in CAD. Both plant-based and seafood-based omega-3s showed these effects (7).
Good sources of omega-3s from plant-based sources include nuts, such as walnuts, and ground flaxseed. Of course, be cautious about consuming too many nuts, since they’re also calorically dense.
Consume a modest amount of chocolate
In an analysis of six studies with over 336,000 participants, researchers found that eating chocolate at least once a week was associated with an 8 percent decreased risk of coronary artery disease when compared with consuming chocolate less than once a week (8).
The author notes that chocolate contains heart healthy nutrients such as flavonoids, methylxanthines, polyphenols and stearic acid which may reduce inflammation and increase good cholesterol. The study did not examine whether any particular type of chocolate is more beneficial or whether there is an ideal portion size.
An earlier study did show that two pieces of chocolate a week may decrease the risk of a heart attack by 37 percent, compared to those who consume less (9).
Both study’s authors warn against the idea that more is better. High fat and sugar content and chocolate’s caloric density may have detrimental effects when consumed at much higher levels.
I typically recommend that patients have one to two squares — about one-fifth to two-fifths of an ounce — of high-cocoa-content dark chocolate daily. Aim for chocolate labeled with 80 percent cocoa content.
You can also get chocolate’s benefits without the fat and sugar by adding unsweetened, cocoa powder to a fruit and vegetable smoothie. Do not use Dutch-process cocoa, also known as alkalized cocoa; the processing can remove up to 90 percent of the flavanols (10).
References:
(1) cdc.gov. (2) Arch Intern Med. 2004 Feb 23;164(4):370-376. (3) nutrition.org (4) NHANES 2009-2010 Data Brief No. 12. Sep 2014. (5) eatright.org. (6) Arch Intern Med. 2001 Nov 26;161(21):2573-2578. (7) Circulation. 2005 Jan 18;111(2):157-164. (8) Eur J Prev Cardiol. 2021 Oct 13;28(12):e33-e35. (9) BMJ 2011; 343:d4488. (10) J Agric Food Chem. 2008 Sep 24;56(18):8527-33.
Dr. David Dunaief is a speaker, author and local lifestyle medicine physician focusing on the integration of medicine, nutrition, fitness and stress management. For further information, visit www.medicalcompassmd.com or consult your personal physician.
Gurwin‘s Immersion Room honored at McKnight’s Excellence in Technology Awards competition
Gurwin Healthcare System in Commack recently announced that its Immersion Room for Memory Care has won Gold in the Resident Engagement & Recreation category, and “Best in Show” in the 14th Annual McKnight’s Excellence in Technology Awards competition.
The annual industry competition recognizes healthcare organizations that demonstrate excellence in the development and implementation of cutting-edge technologies that positively impact the aging services sector.
Located in the heart of Gurwin Jewish Nursing & Rehabilitation Center’s Memory Care Unit (MCU), the Immersion Room is the first of its kind in long-term care on Long Island, designed specifically for Alzheimer’s and dementia patients, and was created in collaboration with Besser Rooms of Amityville. Gurwin’s Immersion Room incorporates state-of-the-art projector technology and custom-made immersive experiences with stimulating sights, sounds and scents to engage the senses, mitigate symptoms and stir memories from bygone days. The innovative technology helps connect residents with parts of themselves that – in some cases – have been lost for years.
“We are deeply honored to receive this recognition for the Gurwin Immersion Room, which is a testament to our commitment to enhancing the quality of life for our residents living in our Memory Care Unit,” said Stuart B. Almer, President and CEO of Gurwin Healthcare System. “The rapid growth of an aging population, together with the rising number of people affected by Alzheimer’s Disease and other cognitive issues has brought an urgent need for effective support therapies to ease symptoms of these diseases. We continually seek out advanced technologies and innovations that will help our residents feel more comforted and connected as they navigate their care journey.”
Made possible through a grant from the Alzheimer’s Foundation of America, Gurwin’s Immersion Room is at its core an augmented virtual reality reminiscence therapy program, sans cumbersome VR googles, offering an engaging multisensory experience. The patented wall system is integrated with custom software designed to create therapeutic user experiences in a safe and stimulating environment. The total experience includes a seamless projection of 4K video onto each wall, surround sound, an aromatherapy feature and custom-made props, enabling residents to become fully immersed in the experience selected. From calming scenes customized to match resident interests such as a snowy forest or quiet chair yoga, or a more lively experience with a hands-on virtual drive through Gurwin park, or a YouTube roller coaster experience, the Gurwin Immersion Room offers a high-tech, holistic means to ease dementia symptoms, preserve cognitive function and enhance quality of life.
Piloting the program at Gurwin is Kathleen Biggs, CTRS, a Certified Dementia Specialist and Gurwin’s Assistant Director of Therapeutic Recreation, who says that the Immersion Room has enhanced programming for residents on the 60-bed Memory Care Unit. “The Immersion Room delivers individualized, patient-centric experiences that resonate with our residents and offer opportunities that may never have been possible again. Since its inception, we’ve noted sustained engagement in the experience provided, positive reminiscing and reduction in negative behaviors for those participating in the experiences. The Immersion Room is a holistic, non-pharmacological intervention that is helping to create meaningful connections and experiences for Gurwin’s memory care residents and their families to share.”
Click here to see a video on the Immersion Room: https://www.youtube.com/watch?v=G5nklDERdQ0
About Gurwin Healthcare System
Gurwin Healthcare System is a renowned healthcare provider offering a full continuum of healthcare and senior living services for more than 35 years. Set on a 36-acre campus in Commack, NY, the System includes Gurwin Jewish Nursing & Rehabilitation Center, providing short-term rehabilitation and long-term skilled nursing care, memory care, respiratory and ventilator care, palliative and hospice care, social and medical adult day programs and on-site dialysis. Located within the Center is Gurwin Home Care agencies which provide in-home skilled care as well as home health aides. Sharing the campus is Gurwin’s Assisted Living community, Gurwin Jewish ~ Fay J. Lindner Residences, and Fountaingate Gardens, a luxury apartment independent living community. Completing the Gurwin family of healthcare services is Island Nursing and Rehab Center, a 120-bed skilled nursing facility located in Holtsville, New York. For more information, visit www.gurwin.org. Follow Gurwin on Facebook (@GurwinNursingRehab) (@GurwinAssistedLiving) and on X (@GurwinJewish).
About the McKnight’s Excellence in Technology Awards
Recognizing healthcare organizations that have effectively utilized technology to enhance care and operations within their facilities, the McKnight’s Tech Awards honors organizations that are revolutionizing the industry within three divisions: Senior Living, Skilled Nursing, and Home Care. Each division for this competition was divided into four categories: Quality, Innovator of the Year, Keep It Super Simple, and Building Bridges. Submissions were judged by a distinguished, independent panel of 21 long-term care stakeholders.
Gurwin Adult Day Care Health Program hosts inspiring Art Gala for their program artists
Gurwin Jewish Nursing & Rehabilitation’s Adult Day Care Health Program recently hosted an Art Gala, celebrating the artistic achievements of their program participants. The event showcased their creativity and talents in a stunning display of more than 50 pieces of artwork, ranging from mixed media to pottery and jewelry.
The Program’s main lobby and hallway were transformed into a captivating gallery, featuring acrylic paintings on canvas, watercolors, colored pencil drawings, marker illustrations and an impressive selection of handcrafted pottery and jewelry. Visitors admired the diverse styles and expressions that reflected the enthusiasm and talent of each artist.
In March 2025, selected pieces from Gurwin’s Adult Day Care Health Program’s gala will be showcased in the Commack Public Library’s gallery, bringing this remarkable exhibit to the wider local community.
Significant to the event’s success is art mentor Marcia Tapia, who runs the Love Without Barriers Foundation. For the past two years, Marcia has generously volunteered her time every Thursday morning, guiding Gurwin’s Adult Day Care participants with compassion, patience and exceptional teaching skills. Through her mentorship, participants have gained confidence and refined their artistic techniques, unlocking their creative potential.
The Art Gala also included a heartfelt tribute to one of the program’s most talented artists, Olga Trujillo. Olga’s artwork holds a special place in the program, with one of her pieces featured as the cover of the 2024 Alzheimer’s Disease Resource Center’s Annual Calendar. All of Olga’s works were beautifully displayed at the event, honoring her memory.
“Our art program is one of the many awe-inspiring activities our participants engage in,” said Jeraldine Fedoriw, LMSW, Chief Adult Day Officer at Gurwin. “We’ve had legally blind individuals create stunning artwork, even when they’ve never done any type of art before. Our Art Gala highlighted their pride in showing their work and the appreciation of their families says it all.”
Attendees left inspired by the passion of the artists from the Gurwin Adult Day Care Program.
# # #
About Gurwin Adult Day Care Program:
The Gurwin Adult Day Care Program, located at Gurwin Jewish Nursing & Rehabilitation Center, is part of the Gurwin Healthcare System and offers a compassionate and supportive environment for individuals in need of daytime care. Designed for seniors and adults with chronic illnesses or disabilities, the program focuses on enhancing quality of life through medical supervision, personalized care plans and engaging activities. Participants receive tailored services, including physical therapy, socialization opportunities, and cognitive stimulation from a team of skilled professionals dedicated to meeting both the medical and emotional needs of participants. The award-winning program is located in Commack, NY, and serves the surrounding communities. For more information, please visit www. gurwin.org/adult-day-health or call 631-715-2520.
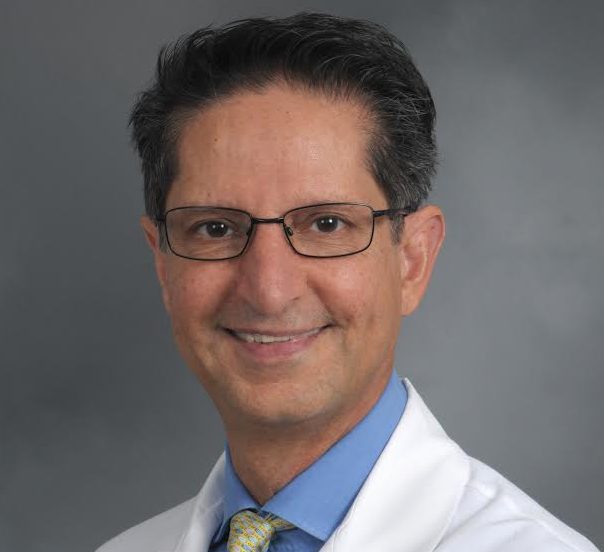
Dr. Farzad Forohar joins Stony Brook Medicine Physician Network in Smithtown
Dr. Forohar is a highly respected, board-certified gastroenterologist with more than 25 years of experience. He has been a dedicated healthcare provider to the Smithtown and surrounding communities, offering compassionate and comprehensive care to his patients.
“We are thrilled that Dr. Forohar has joined Stony Brook Medicine Community Medical Group,” said Dr. Olga Aroniadis, Chief of Gastroenterology and Hepatology at Stony Brook Medicine. “Dr. Forohar’s partnership enables Stony Brook Medicine Gastroenterology to continue to expand its footprint, allowing us to seamlessly service our community and provide exceptional care to our patients.”
Dr. Forohar received his medical degree from the University of Pécs Medical School in Pécs, Hungary. He then completed his internal medicine residency and gastroenterology fellowship at Montefiore Medical Center in Bronx, New York.
Reflecting on his journey, Dr. Forohar shared, “I have had the pleasure of living in and serving this community for the past 25 years. As my practice has grown and evolved, so has Stony Brook University. Becoming what it is today: a world-class hospital system. By joining Stony Brook Medicine, my patients’ needs are best served right here at home.”
Patients who wish to make an appointment with Farzad Forohar, MD, should call 631-724-5300.
Medical Compass: Strategies to save your vision
Diabetes complications can include permanent vision loss
By David Dunaief, M.D.

Diabetic retinopathy (DR) is the leading cause of blindness among U.S. adults, ages 20 to 74 years old (1). As the name implies, it’s a follow-on to diabetes, and it occurs when the blood vessels that feed the light-sensitive tissue at the back of your eye become damaged. It can progress to blurred vision and blindness, typically affecting both eyes.
As of 2023, only about 66 percent of adults with diabetes had a recommended annual eye screening (2). Why is this important? Because the earlier you catch it, the more likely you will be able to prevent or limit permanent vision loss with treatments that target its early stages.
A consequence of DR can be diabetic macular edema (DME) (3). With DME, swelling of the macula, which is an oval spot in the central portion of the retina, can cause significant vision loss. Those with the longest duration of diabetes have the greatest risk for DME.
Unfortunately, the symptoms of vision loss often don’t occur until the later stages of the disorder, after it’s too late to reverse the damage.
How do you treat diabetic macular edema?
DME treatments often include eye injections of anti-VEGF medications, either alone or alongside laser treatments. They work by inhibiting overproduction of a protein called vascular endothelial growth factor (VEGF) (4). These can slow the progression of DME or reverse it (4).
The results from a randomized controlled trial showed that eye injections with ranibizumab (Lucentis) in conjunction with laser treatments, whether laser treatments were given promptly or delayed for at least 24 weeks, were effective in treating DME (5).
Other treatments can include NSAID and/or steroid drops that attempt to reduce swelling of the macula.
Can you reduce DME risk by treating diabetes?
Unfortunately, medications that treat type 2 diabetes do not lower your risk of DME. The THIN trial, a retrospective study, found that a class of diabetes drugs, thiazolidinediones, which includes Avandia and Actos, actually increased the occurrence of DME compared to those who did not use these oral medications (6). Those receiving these drugs had a 1.3 percent incidence of DME at year one, whereas those who did not had a 0.2 percent incidence. This persisted through the 10 years of follow-up. In addition to DME occurrence, the FDA warns of other significant side effects from these drugs.
To make matters worse, of the 103,000 diabetes patients reviewed, those who received both thiazolidinediones and insulin had an even greater incidence of DME. It was unclear whether the findings were caused by the drugs or by the severity of the diabetes, itself.
This contradicts a previous ACCORD eye sub-study, a cross-sectional analysis, which did not show an association between thiazolidinediones and DME (7). This study involved review of 3,473 participants who had photographs taken of the fundus (the back of the eye).
What does this ultimately mean? Both studies had weaknesses. It was not clear how long the patients had been using the thiazolidinediones in either study or whether their sugars were controlled and to what degree. The researchers were also unable to control for all other possible confounding factors (8). There are additional studies underway to clarify these results.
Can glucose control and diet change the equation?
The risk of progression of DR was significantly lower with intensive blood sugar controls using medications, one of the few positive highlights of the ACCORD trial (9). Unfortunately, medication-induced intensive blood sugar control also resulted in increased mortality and no significant change in cardiovascular events. However, an inference can be made: a nutrient-dense, plant-based diet that intensively controls blood sugar is likely to decrease the risk of diabetic retinopathy and further vision complications (10, 11).
If you have diabetes, the best way to avoid DR and DME is to maintain effective control of your sugars. It is also crucial that you have a yearly eye exam by an ophthalmologist. This will help detect issues early, before permanent vision loss occurs. If you are taking the oral diabetes class thiazolidinediones, this is especially important.
References:
(1) cdc.gov. (2) odphp.health.gov. (3) mayoclinic.org. (4) Community Eye Health. 2014; 27(87): 44–46. (5) ASRS. Presented 2014 Aug. 11. (6) Arch Intern Med. 2012;172:1005-1011. (7) Arch Ophthalmol. 2010 March;128:312-318. (8) Arch Intern Med. 2012;172:1011-1013. (9) www.nei.nih.gov. (10) OJPM. 2012;2:364-371. (11) Am J Clin Nutr. 2009;89:1588S-1596S.
Dr. David Dunaief is a speaker, author and local lifestyle medicine physician focusing on the integration of medicine, nutrition, fitness and stress management. For further information, visit www.medicalcompassmd.com or consult your personal physician.
Mather Hospital dedicates new Outpatient Behavioral Health building

Northwell’s Mather Hospital in Port Jefferson formally dedicated its recently acquired Outpatient Behavioral Health Services building that allows the hospital to transform how it provides mental health services at a ribbon cutting ceremony on Nov. 25.
The building, located across the street from the hospital at 100 Highlands Blvd., was purchased with public and private funding totaling $9.2 million including a grant from the NYS Department of Health.
“Tonight, we choose hope. Tonight, we celebrate a victory,” Erin Dainer, MD, Chair of the Department of Psychiatry for Mather Hospital, said at the ribbon-cutting ceremony. “This facility, born from the collective will of government, healthcare providers, and generous philanthropists, stands as proof that together, we can make a difference. Within these walls, lives will be transformed.”
The building houses Mather’s Adult and Adolescent Partial Hospitalization Programs, Chemical Dependency Program, Eating Disorders and Gambling Addiction programs, and a new Rapid Access Center allowing patients immediate access to assessments and referrals for behavorial health care. The Center is expected to be opened by the end of the year.
As part of the acquisition, Mather also expanded its Adolescent Partial Hospitalization program by 10 slots and added a co-occurring disorders track. The hospital also added capacity for its outpatient Medication Assisted Treatment program.
A recent series of community leader forums conducted by the hospital revealed a severe shortage of behavioral health services for both adolescents and adults was a top concern.
“The statistics are stark, but they are not just numbers. They represent real people, our friends, family, and neighbors. Every year, more than one in five New Yorkers battle the invisible wounds of mental health disorders, and in any year one in ten face challenges so profound they impact their ability to work, to love, to simply live,” said Dr. Dainer. “The need is monumental and has only been made worse by the opioid epidemic and recent pandemic.”
“There is no doubt we have a mental health and substance abuse crisis in this country,” said Denise Driscoll, NP, Assistant Vice President for Behavioral Health at Mather Hospital, noting that 53 million Americans are living with mental illness. “Suicide is the 2nd leading cause of death among people aged 10-14 and the 12th leading cause of death overall in the U.S, and 2.5 million Americans are diagnosed with an opioid use disorder. According to the CDC, annual drug overdose deaths have eclipsed the peak of yearly deaths from car crashes, gun violence or any one year of the AIDS epidemic.”
Driscoll said that there is only one provider available for every 350 individuals looking for services, and 28% of adults experiencing mental health symptoms reported they were not able to access or navigate their way to the treatment they so desperately needed.
“Let 100 Highlands be a permanent symbol to our community that no one gets left behind and a beacon of hope to those living with mental illness and substance abuse that recovery and a life well lived is possible,” she said.
SBU News: Nurse clinician and educator named to new SUNY Nursing Simulation Fellowship
Debra Giugliano, RN, PhD, a Clinical Assistant Professor in the Stony Brook University School of Nursing, was recently selected by the State University of New York (SUNY) to be a member of the inaugural class of the SUNY Nursing Simulation Fellowship, an initiative for the 2024-25 academic year that will further advance all SUNY nursing programs to adopt simulation-based education for students.

Announced by the SUNY Chancellor John B. King Jr., the Fellowship is also part of a larger effort to prepare more nurses for New York State’s health care workforce – a major objective of Governor Kathy Hochul and SUNY. It was developed based on recommendations from the SUNY Future of Health Care Workforce Task Force, a group organized to guide SUNY in addressing the critical health care workforce shortage and Governor’s goal of increasing this workforce in NYS by 20 percent. Nursing simulation is one of four priority areas identified by the Task Force.
The 11 Fellows of the inaugural class will advance their knowledge and skills in simulation training by completing a six-month continuing education and simulation training program, attending monthly virtual meetings and in-person retreats on the topic led by SUNY, and attend the International Meeting on Simulation Healthcare from January 10-14 in Orlando, Fla.
As of May 2023, SUNY nursing students can complete as much as one-third of their clinical training through simulation education.
“We are excited for the School of Nursing and for Dr. Giugliano with her selection for this inaugural Nursing Simulation Fellowship,” said Pat Bruckenthal, RN, PhD, Dean of the Stony Brook University School of Nursing. “This opportunity will enable Dr. Giugliano to bring our student learning experiences to the forefront of innovation and impact the preparation of our next generation of nurse leaders.”
A long-time clinician and educator in the School of Nursing and a resident of St. James, Giugliano is a certified pediatric nurse practitioner and pediatric oncology nurse. Her clinical specialties include caring for children with cancer and blood disorders in both inpatient and outpatient settings. The recipient of numerous awards in nursing clinical care and training, Giugliano is also the Founder and Director of the internationally recognized School Intervention and Reentry Program at Stony Brook Children’s Hospital.
“I am honored to have been chosen for this Fellowship and look forward to gaining the necessary expertise to elevate nursing simulation and create a nursing simulation network within SUNY,” said Giugliano.
She and other fellows will have the unique opportunity to shape the future of simulation-based learning across the SUNY system. Through their expertise, they will contribute to the development of the SUNY Simulation Shared Resource Library, a central repository of nursing simulation resources that will benefit nursing education programs system-wide.
Captions:
Simulation training in Stony Brook’s School of Nursing is an integral aspect of clinical education in the future workforce.
Credit: Jeanne Neville, Stony Brook Medicine
Debra Giugliano, RN, PhD
Credit: Jeanne Neville, Stony Brook Medicine