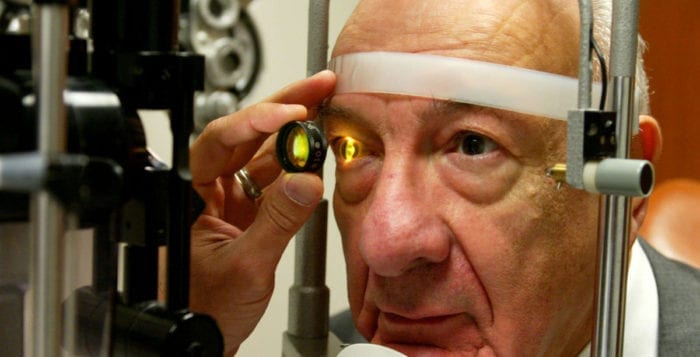
Common medications may affect vision
By David Dunaief, M.D.

When we refer to adverse events with medications, we usually focus on systemic consequences. However, we rarely address the fact that eyes can be adversely affected by medications. There have been several studies that illustrate this very important point.
It is vital that we recognize the symptoms of eye distress. Some of these may indicate ophthalmic emergencies. The medications studied include common therapeutics, such as bisphosphonates, aspirin, a class of antibiotics called fluoroquinolones and a migraine therapy. I will explain the symptoms to be cognizant of with each.
The impact of bisphosphonates
The class of drugs known as bisphosphonates is a mainstay for the prevention and treatment of osteoporosis. Adverse news about bisphosphonates typically focuses on atypical femur fractures and osteonecrosis (death of part of the jawbone), not on an ocular effect. However, in a large retrospective study (looking at past data), oral bisphosphonates were shown to increase the risk of uveitis and scleritis, both inflammatory eye diseases, by 45 and 51 percent, respectively (1). One out of every 1,100 patients treated with the drugs suffered from uveitis, and one out of every 370 patients treated suffered from scleritis.
Why is this important? The consequences of not treating uveitis can lead to complications, such as glaucoma and cataracts. The symptoms of uveitis typically include eye redness, pain, light sensitivity, decreased vision and floaters (2).
For scleritis, the symptoms are severe pain that radiates to the face and around the orbit, with worsening in the evening and morning and with eye movements (3). Uveitis affects the iris and ciliary body (fluid inside the eye and muscles that help the eye focus), while scleritis affects the sclera, or white part of the eye.
These adverse eye events occurred only in first-time users. The authors believe the mechanism of action may involve the release of inflammatory factors by the bisphosphonates.
Aspirin yet again, maybe not?
It seems aspirin can never get a break. It has been implicated in gastrointestinal bleeds and hemorrhagic (bleeding) strokes. The European Eye Study also suggests that aspirin increases the risk of age-related macular degeneration (4). The primary effect is seen, unfortunately, with wet AMD, which is the form that leads to central vision loss. The risk of wet AMD is directly related to the frequency of aspirin use. When aspirin is used at least once a week, but not daily, the risk is increased by 30 percent.
But, this is not the complete story. The researchers found that there was no increase in wet AMD in patients over 85 years old. They also found that the potential for angina (chest pain) and cardiovascular deaths was not eliminated.
This study was large and retrospective in design, and it included fundoscopic (retinal) pictures, making the results more reliable. The authors recommend that AMD patients not use aspirin for primary prevention, meaning without current cardiovascular disease. However, aspirin use for secondary prevention — for those with heart disease or a previous stroke — the benefits of the medication outweigh the risks.
In fact, the Physician Health Study, a randomized controlled study published in 2001, found that aspirin may even reduce the risk of AMD (5). In yet another study, the Age Related Eye Disease Study (AREDS), aspirin seemed to have a protective effect when it came to AMD (6). Therefore, please do not stop taking aspirin if you have cardiovascular disease since the results, at best, are mixed when it comes to AMD.
However, what is more relevant is that aspirin has been shown to reduce the risk of vascular mortality by 15 percent, stroke by 25 percent and overall mortality by 10 percent (7). While the jury is still out on the effect of aspirin on AMD, there is the ASPREE-AMD study that was started in 2017 to help answer the question of low-dose aspirin’s, 100 mg daily, impact on AMD risk.
The role of antibiotics: fluoroquinolones in retinal detachment
Fluoroquinolones may have toxic effects on the synthesis of collagen and on connective tissue, potentially resulting in retinal detachments and Achilles tendon rupture. This is a common class of antibiotics used to treat acute diseases, such as urinary tract infections and upper respiratory infections.
In an epidemiologic study, these drugs were shown to increase the risk of retinal detachment by 4.5 times (8). Common fluoroquinolones include ciprofloxacin (Cipro), levofloxacin (Levaquin) and gatifloxacin (Tequin). Although it sounds like an impressive number, it’s not a common occurrence. It takes the treatment of 2,500 patients before one patient is harmed. Also, this was only noticed in current users, not in recent or past users. However, it is a serious condition.
Retinal detachment is an ophthalmic emergency, and patients need to be evaluated by an ophthalmologist urgently to avoid irreparable damage and vision loss. Retinal detachments are treatable with surgery. Best results are seen within 24 hours of symptoms, which include many floaters, bright flashes of light in the periphery and a curtain over the visual field (9). Fortunately, retinal detachments usually only affect one eye.
Migraine medication
Topiramate (Topomax) is a drug used to treat and prevent migraines. In a case-control (with disease vs. without disease) study, topiramate increased the risk of glaucoma in current users by 23 percent. The risk more than doubled to 54 percent in first-time users (10). The mechanism of action may be related to the fact that topiramate increases the risk of intraocular pressure.
It is important to be aware that medications not only have systemic side effects, but ocular ones as well. Many of these medications cause adverse effects that require consultation with an ophthalmologist, especially with aspirin, since the cardiovascular benefits seem to outweigh any negative impacts on AMD with people who have cardiovascular disease. If you have ocular symptoms related to medications, contact your physician immediately.
References:
(1) CMAJ. 2012 May 15;184(8):E431-434. (2) www.mayoclinic.org. (3) www.uptodate.com. (4) Ophthalmology. 2012;119:112-118. (5) Arch Ophthalmol. 2001;119:143-149. (6) Medscape.com. (7) Lancet. 2009;373:1849-1860. (8) JAMA. 2012;307:1414-1419. (9) www.ncbi.nlm.nih.gov. (10) Am J Ophthalmol. 2012 May;153(5):827-830.
Dr. Dunaief is a speaker, author and local lifestyle medicine physician focusing on the integration of medicine, nutrition, fitness and stress management. For further information, visit www.medicalcompassmd.com or consult your personal physician.