Being a hospital patient for any length of time is not likely an experience that engenders tranquility or inner peace for most, but local artists and hospital staff are doing their best to change that.
The 3 North Patient Care Unit at Port Jefferson’s John T. Mather Memorial Hospital, a newly constructed intermediate care unit on the third floor, is now furnished with paintings from artists who donated their work to be displayed for and enjoyed by patients and staff.
The hospital hosted a reception to thank the artists, including Irene Ruddock, president of Setauket Artists, who played a leadership role in getting the idea off the ground.
“The art installation endeavor was the inspiration of Dr. Shug-Hong Young, a cardiologist at Mather Hospital, who purchased one of my paintings which he donated to the hospital’s newest wing,” Ruddock said.
She said Young then took the idea to Mather president, Kenneth Roberts, who liked the concept and requested works featuring Long Island waterways and boats be displayed.
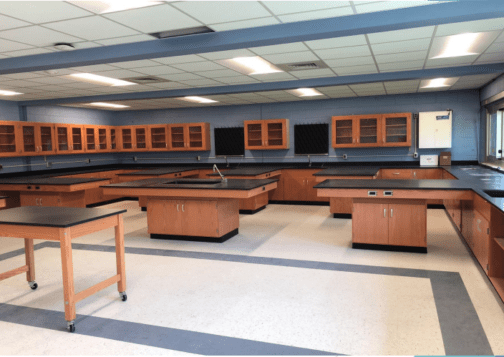
“This is actually a wonderful opportunity and a wonderful meeting of community members and artists with their local community hospital resource,” Roberts said. “We put a brand new wing on with private rooms with computers in the rooms so we don’t have all of the [computers on wheels] or [workstations on wheels] out in the hallways, so nothing is crowded. So we have this brand new nursing station with beautiful finishes, but the one thing we didn’t have was artwork.”
Ruddock was tasked with selecting paintings from her group’s members that fit the bill.
“I chose art that would add to the beauty of the already beautiful space, create a peaceful, serene environment that might provide a sense of spiritual healing,” she said. “I wanted paintings that touch people’s hearts and souls — ones that were memorable and draw you right into the painting.”
Young explained why he donated Ruddock’s initial painting, and why he thought it would brighten up the wing.
“It came to me that if we could bring all of these local artists [works] to the hospital, because many of the artworks reflect local scenes — the beach, the port, the pond — that would make patients feel they are not isolated, they are still connected to the beautiful environment,” he said.
Emily Emma, nurse manager for 3 North who recently transferred to the position, said she asked colleagues in her unit if there was anything she could do to elevate their work and the care they provide to patients, and a common theme emerged in the answers.
“Most of them had said, ‘We would really like some artwork on the walls,’” Emma said. “Patients can’t get enough of them. It’s really a nice peaceful journey to get through their progression of health.”
Jim Molloy, a Miller Place-based artist, was among those who donated a piece to the hospital that he called “Turning Tides.”
“I think that’s what art is about — it’s about brightening up someone’s day,” Molloy said. “If somebody can look at a piece of art and kind of escape for a while, then that makes me feel good, it makes them feel good — it’s perfect.”
Ruddock thanked Roberts, Young and Emma for their efforts in bringing the idea to fruition, as well as Mather employees Nancy Uzo, vice president of public affairs, and Laura Juliano, director of annual giving. Juliano said artist Renée Caine also provided invaluable help during the planning and installation phases of the idea. Caine donated one of her own works.
“By far, the most rewarding aspect of the project was the reaction of the patients, caregivers and staff to the paintings,” Ruddock said. “One staff member said of Michael Kutzing’s painting of a sailing vessel, ‘I mentally take a ride on the boat every day on the Long Island Sound to breathe in the air.’”