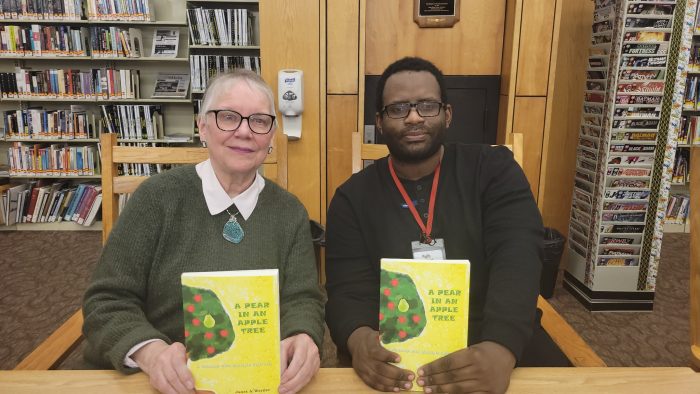
One of TBR News Media’s very own recently embarked on a life-changing collaboration with a former educator.
Kyle Horne, a local artist and frequent contributor of political cartoons and editorial illustrations to our newspapers, has partnered with his former teacher, Janet Werner, to create a book about multiple sclerosis. Together, they tell a moving story of overcoming adversity, revealing a powerful, enduring bond between a student and teacher.
A journey with MS
Werner was diagnosed with multiple sclerosis, commonly known as MS, in 1986. At the onset of her symptoms, she recalled a feeling of numbness in her legs and overwhelming fatigue.
“I actually took off for two weeks from work that first year and just slept,” she said. “I got an MRI at the time, and it showed plaque in the brain, which is white lesions. Depending upon where these white lesions are seen in the brain, it could affect your mobility, cognition and eyesight.”
As the years advanced, Werner’s symptoms gradually progressed. During a startling incident one morning, she temporarily lost her eyesight and hearing completely. “What seemed like hours was about 20 minutes,” she said. “I was terrified because it had never happened before.”
Nearly four decades after her initial diagnosis, Werner explained she is “doing pretty well” despite the heightening symptoms with each passing year. She said managing the symptoms requires plenty of rest and an upbeat mentality.
With husband Ernest, “we try to get some exercise, eat correctly and just keep a positive frame of mind,” she said. “Of course, life is very stressful but we try to be positive.”
‘A Pear in an Apple Tree’
Over several years, Werner wrote “A Pear in an Apple Tree: A Journey with Multiple Sclerosis,” saying she was motivated to write the book for various reasons.
Among them, she noted a lack of public understanding surrounding MS and its symptoms. She also wanted to share her story with those experiencing MS, preparing them for the path ahead and informing them that they are not alone.
“Sometimes with any challenge in your life, you feel like you’re the only one who has this specific condition or challenge, whether it’s MS or cancer and you kind of hide away from the rest of the world,” she said. “That’s not good to do that. I wanted the ‘MSers’ to feel that we’re in this together.”
Werner recalled the moment that gave the book its name. She said she was eating dinner with her husband, struggling with her symptoms that day, when she blurted out, “I feel like a pear in an apple tree, kind of out of place.”
Despite the numerous challenges through the years, Werner said she wrote the book to let others know they have a place with an MS community that also understands their struggles.
A dynamic team
The collaboration between Werner and Horne has been decades in the making. A graduate of Deer Park High School, Horne was her student and a member of the school’s Students Against Destructive Decisions Club, which Werner had advised.‘You have to educate yourself about the disease and how it affects your body. And then learn to adapt.’
— Janet Werner
“He would invite me to some of his book signings and art shows, and we kept in close contact over the years,” she said. “When I was doing this book, I immediately thought of him because I loved his artwork.”
Horne described the early stages of preparing the book with his former teacher. He was eager to sign onto the project.
“She came to me with this idea for a book dealing with MS and how it affects her,” Horne said. Although managing symptoms “can be difficult, those challenges have been very helpful in developing her into the person she is today.”
Along with the cover and back cover, Horne prepared several illustrations throughout the book, tying into the themes of each of its chapters. Together, Werner and Horne developed the characters of Ned and Nancy Neuron.
Through the illustrations he prepared for the book, Horne said he learned much about Werner and her experiences with MS, describing a sense of growth and mutual understanding forged throughout their creative journey together.
“I don’t have MS, but I’m able to sympathize more with Janet and the struggles that she’s had,” the artist said. “She has a very strong spirit when it comes to this.”
An optimistic future
Following the success of their first collaboration, Werner and Horne are already working on the next project, a coloring book that adds an interactive component to the story of Ned and Nancy Neuron.
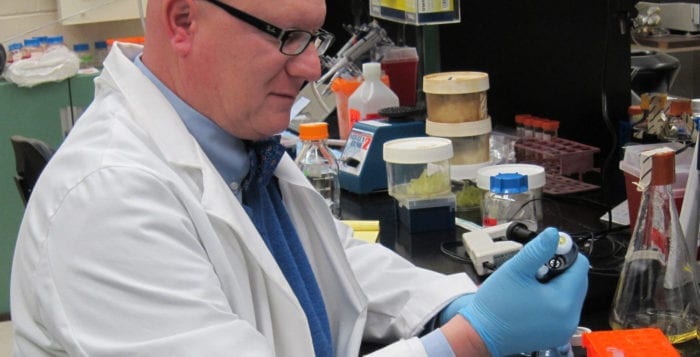
Werner said she remains “very hopeful” that researchers will soon discover a cure for MS. Analyzing the scope of scientific investigation into the condition, she said there is considerable overlap between ongoing MS research and similar autoimmune diseases.
“Research that’s being conducted for, say, AIDS or lupus is also being conducted for MS,” she said. “Stony Brook [University] has an MS center, and their research is going on at a rapid rate. So I am so hopeful.”
Despite the decades she has spent with MS, Werner shares a message of resolve in the face of hardship.
“I think you have to keep fighting,” she said. “You cannot give up. If you’re faced with a challenge, you have to educate yourself about the disease and how it affects your body. And then learn to adapt.”
Horne said the collaboration with Werner has been a personal experience as well. Learning about MS, he said, has informed his outlook on his own life.
“I have a condition known as ulcerative colitis, also known as Crohn’s disease,” Horne said. “Understanding the perspective of another chronic illness, and from a different person, has come to help with my own process and working through my own things.”
He added, “When it comes to something like this it can be very scary at times, but it also can be very rewarding knowing the perseverance of getting through a struggle like that.”
To learn more about MS, visit www.nationalmssociety.org. To purchase “A Pear in an Apple Tree,” visit www.allbook-books.com.