By Daniel Dunaief
People battling cancer can sometimes live long after they and their doctors first start treating the disease. Even if and when their types of cancer don’t continue to threaten their lives in the same way, they can struggle with symptoms such as chronic fatigue, pain, and difficulty sleeping.
These ongoing symptoms, however, could be a remnant of the way the nervous system and cancer interact, as well as a byproduct of the treatment.
Cancer neuroscience uses “tools from both neuroscience and cancer to fundamentally understand how cancer influences the functioning on the nervous system” and how the nervous system can be used to affect cancer, explained Jeremy Borniger, Assistant Professor at Cold Spring Harbor Laboratory.
Indeed, the field of cancer neuroscience, which extends beyond the study and treatment of brain cancer, has been growing over the last six years, after researchers made important discoveries that suggest the possible role and target for treatment of neurons.
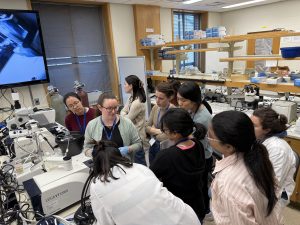
To encourage cancer scientists to learn more about the principles and techniques of neuroscience and to bring neuroscientists up to speed with cancer research, Borniger and three other scientists coordinated the first two-week Methods in Cancer Neuroscience course at Cold Spring Harbor Laboratory last month.
Attended by 14 researchers from domestic and international institutions, the days often started early in the morning and lasted past 10 p.m. The course included lectures about the basic science as well as considerable lab work.
Course attendees, most of whom had a background in cancer biology but little background in neuroscience, appreciated the opportunity to learn from the lecturers and to build their networks.
“We were introduced to a wide variety of techniques from the leading experts in the field and got to listen to insightful lectures from the invited speakers,” said Irem Uppman, a graduate student at Uppsala University in Sweden.
Uppman was grateful for the opportunity to meet her fellow students and hopes to stay in touch throughout their careers.
“It was also very exciting to meet all the instructors and lecturers,” Uppman said. “The small size of the course allowed us to interact more intimately which is something we often can’t do in the setting of big conferences.”
Uppman, who has been a PhD candidate for three years and hopes to graduate in the next two years, is a tumor biologist by background and hopes to incorporate more cancer neuroscience in her future work.
Course origins
During another conference, Borniger recalled how a group of cancer neuroscientists were discussing the field. One of the speakers suggested the need for a workshop where students could learn techniques from both of these disciplines.
“I raised my hand and said, “Cold Spring Harbor does this all the time,” Borniger said.
The leadership at the lab, including CEO Bruce Stillman, were excited about the possibility and encouraged Borniger to help coordinate the course. After the lab publicized the conference, 67 prospective students submitted applications. The organizers had several marathon zoom sessions to review the applicants.
“We wanted a good spread of earlier career and later career students,” said Borniger.
It would have been possible to fill the course with students conducting research on brain cancer exclusively, but the organizers wanted a broader scientific representation.
Neurons and cancer
As electrically active tissue, neurons play important roles in healthy biology as well as with cancer.
“It’s not just another cell type in the tumor environment,” Borniger explained, adding that nerve cells connect tumors with the central nervous system, which governs all conscious and unconscious systems.
Historically, cancer neuroscience has had two major moments that helped push the field into the mainstream of scientific research.
In a couple of papers between 2010 to 2013, before anyone started using the term “cancer neuroscience,” scientists showed that getting rid of localized sympathetic nerves, which include the kinds of nerves that control the heart rate and blood pressure, can cause breast cancer and prostate cancers to stop growing.
“Everyone assumed the nerves don’t really do anything,” Borniger said. They are “little tiny projections in the tumor. A lot of cancer biologists ignored it” in part because of a paper in the 1960’s that suggested tumor cells were not electrically coupled together. Scientists believed, prematurely and inaccurately, that electrochemical signaling didn’t play a role in cancer.
Then, in 2019, three papers came out around the same time that demonstrated that tumors in the brain can form connections with neurons like normal neurons do. These cancerous cells can integrate with circuits and communicate with each other.
“The level of integration that these cancer cells have with your brain dictates how bad the cancer is,” Borniger said. “If you disconnect the cancer cells from the neurons in your brain, you can make cancer much easier to treat.”
Researchers and pharmaceutical companies are looking for ways to use drugs to slow or stop the cancers.
Some research efforts are trying to block the gap junctions which dramatically reduces the number of cancer cells that receive input.
In breast to brain cancer, scientists are looking to target NMDA receptors, while in brain cancer, they’re targeting AMPA receptors.
Researchers are hoping to repurpose drugs approved for other conditions, such as bipolar disorder or epilepsy.
Origin story
When Borniger was in graduate school at Ohio State University, he was interested in sleep and how sleep works. He had the opportunity to attend several lectures and talks to gather information and pursue research that interested him.
In one meeting, which he said he might have attended to get free food, oncology nurses were talking about the subjective experience of cancer patients. At the end of the talk, they shared a summary slide of the top complaints, which included fatigue, pain, sleep disruption, cognitive impairment and changes in appetite.
Borniger thought these were all neuroscience problems.
He immediately looked online to see if anyone had seen how a tumor influences these neurological processes.
When he tested to see if breast cancer could influence brain activity and lead to sleep disruption, what he found convinced him it was a research field worth pursuing.
“The signal that comes from the tumor can reprogram your brain,” he said. “How does that work? That got me into the field.”
When he got the job at CSHL in 2019, Borniger attended a Banbury conference where the top people in the developing field gathered. He’s also interested in the opportunity to contribute to a new field.
“There’s not 30 years of dogma that we’re going to have to break down,” Borniger said. “We’re inventing the foundation as we go.”
Borniger is hoping to continue to expand the field to newer people, including those who work in neurodevelopment, bioinformatics and behavioral science.
The tide is turning towards cancer neuroscience, Borniger believes. Years ago, cancer biologists would say, “Who cares about sleep? We’re driving to cure the cancer!” Now, with help from patient advocates, Borniger explained, clinicians are starting to realize the subjective health of the patient can have “immense impact” on their prognosis.