Non-clinical readings may paint a more complete picture of your risks
By David Dunaief, M.D.

Nearly 120 million U.S. adults, just under half of the population, have hypertension (1). Of these, only 25 percent have successfully controlled their blood pressure to less than 130/80 mmHg, the high end of “normal” blood pressure.
For the remaining 75 percent, the risk of complications, including cardiovascular events and mortality, is significantly higher.
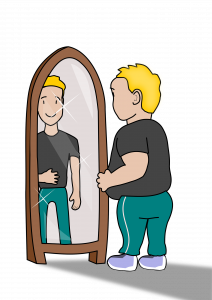
What increases our risk of developing hypertension? An observational study involving 2,763 participants showed that the top three influencers on the risk of developing high blood pressure were poor diet, modest obesity, and cigarette smoking, all of which are modifiable (2).
What increases your risk of complications?
Being significantly overweight or obese, smoking, poor diet, lack of exercise, family history, age, increased sodium, depression, diabetes, low vitamin D, and too much alcohol all increase your risk (3).
The good news is that you can improve your risk profile (4).
What is the effect of gender?
One of the most concerning complications of hypertension is cardiovascular disease. A large observational study with a 31-year duration found that isolated systolic (top number) hypertension increased the risk of cardiovascular disease and death in both men and women between 18 and 49 years old, compared to those who had optimal blood pressure (5). These complications were not affected by onset age.
When the results were sorted by gender, women experienced the greatest effect, with a 55 percent increased risk of cardiovascular disease and 112 percent increased risk of heart disease death.
When to measure your blood pressure
Most of us have our blood pressure measured when we’re at a doctor’s office. While measuring blood pressure in a clinic can be useful, a meta-analysis of nine studies showed that high blood pressure measured at nighttime was potentially a better predictor of myocardial infarctions (heart attacks) and strokes, compared to daytime and clinic readings (5).
For every 10 mmHg rise in nighttime systolic blood pressure, there was a corresponding 25 percent increase in cardiovascular events. The nighttime readings were achieved using 24-hour ambulatory blood pressure measurements (ABPM).
A factor that might increase the risk of nighttime cardiovascular events is masked uncontrolled hypertension (MUCH). MUCH occurs in those who are well-controlled during clinic readings for blood pressure; however, out-of-clinic readings indicate their blood pressure is uncontrolled.
A study of 167 patients found that medication non-compliance was not a significant factor in those experiencing MUCH (6). Of the participants experiencing MUCH, 85.2 percent were fully adherent with their prescribed medications, a number similar to the group that did not experience MUCH.
Interestingly, in the Spanish Society of Hypertension ABPM Registry, MUCH was most often seen during nocturnal hours (7). The study’s authors suggest that ABPM may be a better way to monitor those with higher risk factors for MUCH, such as those whose pressure is borderline in the clinic and those who are smokers, obese or have diabetes.
A previous study of patients with chronic kidney disease (CKD) and hypertension suggested that taking at least one antihypertensive medication at night may be more effective than taking them all in the morning (8). Those who took one or more of their blood pressure medications at night saw a two-third reduction in cardiovascular event risk.
Blueberries and blood pressure
Diet plays an important role in controlling high blood pressure. Lowering sodium is critically important, but adding berries may also be beneficial.
In a study of post-menopausal women with pre-hypertension or stage one hypertension, daily consumption of 22 grams of blueberry powder, the equivalent of one cup of fresh blueberries, reduced systolic blood pressure by a respectable 7 mmHg and diastolic blood pressure by 5 mmHg over two months (9).
This addition of a modest amount of fruit had a significant impact. Blueberries increase nitric oxide, which helps blood vessels relax and reduces blood pressure. While the study used blueberry powder, an equivalent amount of real fruit might lead to an even greater reduction.
High blood pressure and possible cardiovascular complications can be scary, but lifestyle modifications, such as making dietary changes and taking antihypertensive medications at night, can reduce your risks.
References:
(1) millionhearts.hhs.gov. (2) BMC Fam Pract 2015;16(26). (3) uptodate.com. (4) Diabetes Care 2011;34 Suppl 2:S308-312. (5) J Am Coll Cardiol 2015;65(4):327-335. (6) Hypertension. 2019 Sep;74(3):652-659. (7) Eur Heart J 2015;35(46):3304-3312. (8) J Am Soc Nephrol 2011 Dec;22(12):2313-2321. (9) J Acad Nutr Diet 2015;115(3):369-377.
Dr. David Dunaief is a speaker, author and local lifestyle medicine physician focusing on the integration of medicine, nutrition, fitness and stress management. For further information, visit www.medicalcompassmd.com or consult your personal physician.












 By now, most of us have been hit over the head with the fact that too much salt in our diets is unhealthy. Still, we respond with “I don’t use salt,” “I use very little,” or “I don’t have high blood pressure, so I don’t have to worry.” Unfortunately, these are myths. All of us should be concerned about salt or, more specifically, our sodium intake.
By now, most of us have been hit over the head with the fact that too much salt in our diets is unhealthy. Still, we respond with “I don’t use salt,” “I use very little,” or “I don’t have high blood pressure, so I don’t have to worry.” Unfortunately, these are myths. All of us should be concerned about salt or, more specifically, our sodium intake.




