When Jean Noschese’s left hand started to go numb, she didn’t expect her doctor’s visit to lead to brain surgery at Huntington Hospital, where she met Dr. Robert Kerr, a neurosurgeon who had a new way of operating on the brain.
On Oct. 16, 2013, Noschese experienced a head-on collision while driving in Hauppauge. The car accident left her in need of several surgeries, including ones to repair her rotator cuff and replace her hip. But it was when she started losing sensation in her left hand, in 2014, that she went to a specialist. Noschese, who initially wondered if her issue with her hand was related to her crash, was rushed to the hospital after her hand specialist thought Noschese was experiencing a stroke.
But instead of a stroke, the doctors found a three-by-four-centimeter lesion on the right side of her brain that caused paralysis on the left side of her body. Her lesion wasn’t caused by the crash, but from Noschese’s breast cancer that had metastasized to her brain. Noschese was diagnosed with breast cancer in 2005.
Doctors wanted to perform brain surgery the following day, on Dec. 22, 2014, according to Noschese,
“It’s overwhelming to hear that you need brain surgery,” she said.
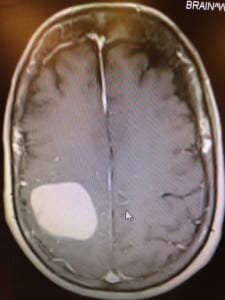
But Kerr, who met with Noschese when she entered the hospital, reassured her and reviewed the procedure with her. A new brain-mapping technique, using the Synaptive Medical’s BrightMatter Plan product, involves several new tools, including a highly engineered tube that splits brain tissue fibers and allows neurosurgeons to access difficult and deep parts of the brain easily. The procedure also utilizes a fiber optic, high definition telescope that creates a “cone of visualization” that allows surgeons to clearly view all planes of the brain they are working on.
The technique also features a procedure called the myriad, which uses a blunt suction device that peels off tumors from dangerous or sensitive areas without damaging surrounding areas in the brain.
“Traditionally, surgeries for deeper regions actually involve destroying a certain amount of tissue to get to the target area,” Kerr said.
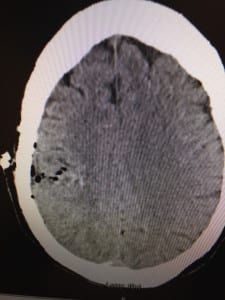
According to Kerr, in traditional brain surgeries, metal retractors are used to create a pathway so surgeons can access target areas of the brain. Doctors use the retractors to pull the edges of the brain apart and create a pathway.
Kerr said the issue with this technique is that, regardless of how careful a surgeon is, he or she may still push on these retractors, which widens the pathway the surgeon created from surface of the brain to the target area. As a result, the patient is left with a hole in part of the brain, which means the patient will take longer to recover from the surgery.
Stony Brook Medicine Neurosurgeon Dr. David Chesler said Synaptive Medical’s BrightMatter Plan procedure is only appropriate under certain circumstances.
“Tumors that come right to the surface, where they’re easily approachable, I don’t think there’s any benefit to using this technique, because the tumor is right there,” Chesler said. Chesler took a course for the procedure about two years ago. While he thinks the technique is beneficial, he does not think it is a be-all and end-all procedure for brain surgery.
While the procedure is minimally invasive, may decrease the chance of injuring the patient during the operation and allows surgeons to approach lesions or blood clots, Chesler said there are some downsides to the technique. He said that the technology of this technique is not new, but simply creates a new system that makes it easier for surgeons to implement.
Additionally, minimally invasive procedures double or triple the length of an operation, depending on the surgeon and the nature of the surgery. Surgeons who may not be very experienced may leave parts of lesions or tumors and blood clots behind because of limited visualization.
Surgeons can only see what is at the end of the tube, which is around the diameter of a dime.
Kerr said this procedure will decrease patients’ recovery time. Patients are usually tired following the surgery and require extensive amounts of rest before they are discharged from the hospital. Noschese, however, was alert and speaking two hours after the surgery. Not only did she regain sensation in her hand, but she was also able to grab and hold onto a variety of objects.
Chesler, like Kerr, said patients who receive traditional surgeries for deep-seated lesions or blood clots can do well. He said his patients’ deficits were more related to the “structures involved with the tumor,” as opposed to the approach used. Chesler has seen both good and bad outcomes from this technique
According to Kerr, few surgeons are using this technique.
“Neurosurgeons are skeptics and slow adopters and I think that’s appropriate,” Kerr said, explaining why more surgeons may stick to traditional brain surgery practices.
While Chesler said the procedure should be used for the right case and with an experienced surgeon, he said staff are looking to adopt this technique at Stony Brook University Hospital. Chesler, who does both pediatric and adult neurosurgery, said he is simply looking for the right case. Recently he hasn’t come across a case that calls for the technique.
Doctors must demonstrate the procedure and illustrate its benefits when introducing the technique to the hospital. Hospitals need to invest in the procedure for a surgeon to officially implement it.
Although Chesler said there are other systems that surgeons can use to reach a similar goal, Kerr said the technique is a glimpse into the future of this type of surgery.
“I think this technology reflects the future of neurosurgery and accessing deep-seated lesions in a kinder, gentler, more precise way,” Kerr said. “I think this is representing a future paradigm shift in the way that brain surgery is done, and I think that we will see many more adopting this in a very short period of time.”





