By Daniel Dunaief
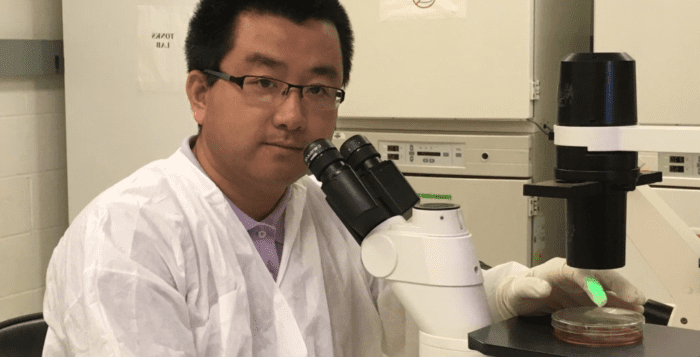
The past can come back to haunt us, even in the world of genetics. Over the course of millions of years, plants and animals have battled against viruses, some of which inserted their genes into the host. Through those genetic struggles, explained Molly Hammell, an assistant professor at Cold Spring Harbor Laboratory, cells develop “elaborate ways to fight back,” even as they continue to make copies of these pieces of DNA.
Sometimes, when our defenses break down, these retrotransposons, or jumping genes, can become active again. Indeed, that appears to be the case in a fly model of amyotrophic lateral sclerosis, also known as ALS or Lou Gehrig’s disease.
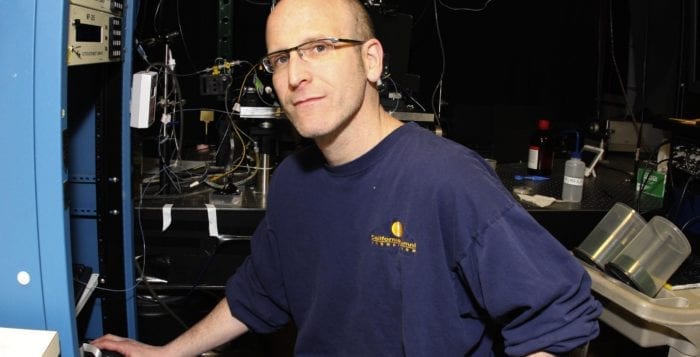
Working on a fruit fly model of ALS, Joshua Dubnau, an associate professor at Stony Brook University, Lisa Krug, who earned her doctorate at Cold Spring Harbor Laboratory and is now working at Kallyope in New York, and Hammell showed that these ancient genetic invaders play an important role in the disease amid activation by a protein often linked to ALS called TDP-43.
A recent study, published in PLOS Genetics, “really proves that retroviral reactivation (as a consequence of TDP-activity) is … central to either causing or accelerating neuronal cell death when TDP-43 inclusions are present,” explained Hammell in an email. If TDP-43 plays the same role for humans, this would suggest that targeting this protein or the jumping genes, it activates could lead to potential treatment for ALS.
These collaborators showed that an aggregation of this protein turned on jumping genes. These genes can make copies of themselves and insert themselves in other parts of the genetic code. In this case, TDP-43 expression disrupts the normal immune-like system that silences retrotransposons such as gypsy, which is a particular type of jumping gene in the fruit fly.
When gypsy was activated, the fruit fly exhibited many of the features of ALS, including protein pathology, problems with movement, shortened life span and cell death or glia and neurons in the brain. The scientists were also able to turn gypsy off, which improved the health and extended the life span of the fly.
Mimicking this protein results in broad activation of several retrotransposons. If this also occurs in people, the disease may activate a retrotransposon that is the human analog to gypsy, called HERV-K, as well as other retrotransposons. The study also suggests that DNA damage caused by retrotransposons may active a cell suicide mechanism. Finally, this effort showed a means by which the protein disrupts the normal immune surveillance that keeps retrotransposons quiet.
To be sure, Dubnau cautioned that animal models of a disease may not translate when returning to people. Researchers need to look at more patients at all the retrotransposons in the human genome to monitor its prevalence, Dubnau suggested. If the link between retrotransposon activation and the development of ALS is as evident in humans as it is in the fruit fly, scientists may take an approach similar to that which they took to battle the human immuno-deficiency virus, or HIV. Retrotransposons have an RNA genome that needs to be copied to DNA. This, Dubnau explained, is the step in the process where researchers attacked the virus.
In a small subset of HIV patients who have motor neuron symptoms that are similar to ALS, Avi Nath, a senior investigator at the National Institutes of Health discovered that treating patients with the typical HIV medication cocktail helped relieve their ALS symptoms as well.
“What is not known is whether, for some reason, this subset of patients had an ALS syndrome caused by HIV or they were curing them” by treating HIV, Dubnau said. Nath is currently involved in one of two clinical trials to see if HIV medications help ALS patients. The next step for Dubnau and Hammell is to screen the tissue of numerous ALS patients after their death to see if their retrotransposons were elevated.
In addition to NIH funding, the scientists received financial support from Ride for Life, which is a not-for-profit organization started in 1997 that raises funds for research to find a cure for ALS, supports patients and their families through patient services and raises awareness of ALS. Every May, Ride for Life conducts a 12-day, 100-mile patient wheelchair ride across Long Island. Dubnau and Hammell, who received a $300,000 grant from Ride for Life in 2015, said they have been inspired by Ride for Life founder Chris Pendergast.
Meeting Pendergast “has had a big impact,” Dubnau said. “He’s a force of nature. He’s an incredibly strong and intelligent person.” Receiving funds from Ride for Life created a sense of personal obligation to Pendergast and many other people who “had raised that money through sweat and effort.”
Without funding from the Ride for Life Foundation, “We would not have the resources to obtain these samples and do the sequencing experiments necessary to prove that this is a clinically relevant phenomenon in a large number of ALS patients,” Hammell said.
Through an email, Pendergast explained that Ride for Life chose to fund the work by Dubnau and Hammell because the research met several criteria, including that it might lead to new strategies to treat ALS and the research was on Long Island, which is a “powerful affirmation for our generous donors.”
Pendergast emphasized the importance of funding basic ALS research. “We need to know why it develops, how it progresses [and] how it can be diagnosed and monitored,” he urged.
A resident of Huntington, Dubnau and his wife Nicole Maher, who works at the Nature Conservancy as a climate scientist, have a nine-year-old daughter, Caitlin. Reflecting both of her parents’ professional interests, Caitlin is going to a statewide science fair, where she is presenting her work on how temperature affects the life span of insects.
As for his research, Dubnau hopes a further exploration of TDP-43 might reveal an important step in the progression of ALS. He hopes this discovery may suggest a strategy researchers and clinicians can take that might “stop the cascade of events” in ALS.