Key lifestyle choices may reduce your risk significantly
By David Dunaief, M.D.

Happy “Movember!” The Movember Foundation is in its 11th year of raising awareness and research money for men’s health issues (1). What better time to discuss prostate cancer prevention?
The best way to avoid prostate cancer is through lifestyle modifications, which means learning about both detrimental and beneficial approaches. There are a host of things that may increase your risk and others that may decrease your likelihood of prostate cancer. Your family history does not mean you can’t alter gene expression with the choices you make.
What may increase the risk of prostate cancer? Contributing factors include obesity, animal fat and supplements, such as vitamin E and selenium. Equally as important, factors that may reduce risk include vegetables, especially cruciferous, and tomato sauce or cooked tomatoes.
Vitamin E and selenium
In the SELECT trial, a randomized clinical trial (RCT), a dose of 400 mg of vitamin E actually increased the risk of prostate cancer by 17 percent (2). Though significant, this is not a tremendous clinical effect. It does show that vitamin E should not be used for prevention of prostate cancer. Interestingly, in this study, selenium may have helped to reduce the mortality risk in the selenium plus vitamin E arm, but selenium trended toward a slight increased risk when taken alone. Therefore, I would not recommend that men take selenium or vitamin E for prevention.
Obesity
Obesity showed conflicting results, prompting the study authors to analyze the results further. According to a review of the literature, obesity may slightly decrease the risk of nonaggressive prostate cancer, however increase risk of aggressive disease (3). Don’t think this means that obesity has protective effects. It’s quite the contrary. The authors attribute the lower incidence of nonaggressive prostate cancer to the possibility that it is more difficult to detect the disease in obese men, since larger prostates make biopsies less effective. What the results tell us is that those who are obese have a greater risk of dying from prostate cancer when it is diagnosed.
Animal fat, red and processed meats

It seems there is a direct effect between the amount of animal fat we consume and incidence of prostate cancer. In the Health Professionals Follow-up Study, a large observational study, those who consumed the highest amount of animal fat had a 63 percent increased risk, compared to those who consumed the least (4).
Here is the kicker: It was not just the percent increase that was important, but the fact that it was an increase in advanced or metastatic prostate cancer. Also, in this study, red meat had an even greater, approximately 2.5-fold, increased risk of advanced disease. If you are going to eat red meat, I recommend decreased frequency, like lean meat once every two weeks or once a month.
In another large, prospective (forward-looking) observational study, the authors concluded that red and processed meats increase the risk of advanced prostate cancer through heme iron, barbecuing/grilling and nitrate/nitrite content (5).
Omega-3s paradox
When we think of omega-3 fatty acids or fish oil, we think “protective” or “beneficial.” However, these may increase the risk of prostate cancer, according to one epidemiological study (6). This study, called the Prostate Cancer Prevention Trial, involving a seven-year follow-up period, showed that docosahexaenoic acid (DHA), a form of omega-3 fatty acid, increased the risk of high-grade disease 2.5-fold. This finding was unexpected. If you choose to eat fish, salmon or sardines in water with no salt are among the best choices.
Lycopene – found in tomato sauce
Tomato sauce has been shown to potentially reduce the risk of prostate cancer. However, uncooked tomatoes have not shown beneficial effects. This may be because, in order to release lycopene, the tomatoes need to be cooked (7). It is believed that lycopene, which is a type of carotenoid found in tomatoes, is central to this benefit.
In a prospective (forward-looking) study involving 47,365 men who were followed for 12 years, the risk of prostate cancer was reduced by 16 percent (8). The primary source of lycopene in this study was tomato sauce. When the authors looked at tomato sauce alone, they saw a reduction in risk of 23 percent when comparing those who consumed at least two servings a week to those who consumed less than one serving a month. The reduction in severe, or metastatic, prostate cancer risk was even greater, at 35 percent. There was a statistically significant reduction in risk with a very modest amount of tomato sauce.
In the Health Professionals Follow-up Study, the results were similar, with a 21 percent reduction in the risk of prostate cancer (9). Again, tomato sauce was the predominant food responsible for this effect. This was another large observational study with 47,894 participants. Although tomato sauce may be beneficial, many brands are loaded with salt. I recommend to patients that they either make their own sauce or purchase a sauce with no salt, such as one made by Eden Organics.
Vegetable effects
Vegetables, especially cruciferous vegetables, reduce the risk of prostate cancer significantly. In a case-control study (comparing those with and without disease), participants who consumed at least three servings of cruciferous vegetables per week, versus those who consumed less than one per week, saw a 41 percent reduction in prostate cancer risk (10). What’s even more impressive is the effect was twice that of tomato sauce, yet the intake was similarly modest. Cruciferous vegetables include broccoli, cauliflower, bok choy, kale and arugula, to name a few.
When it comes to preventing prostate cancer, lifestyle modification, including making dietary changes, can reduce your risk significantly.
References:
(1) www.movember.com. (2) JAMA. 2011; 306: 1549-1556. (3) Epidemiol Rev. 2007;29:88. (4) J Natl Cancer Inst. 1993;85(19):1571. (5) Am J Epidemiol. 2009;170(9):1165. (6) Am J Epidemiol. 2011 Jun 15;173(12):1429-1439. (7) Exp Biol Med (Maywood). 2002; 227:914-919. (8) J Natl Cancer Inst. 2002;94(5):391. (9) Exp Biol Med (Maywood). 2002; 227:852-859; Int. J. Cancer. 2007;121: 1571–1578. (10) J Natl Cancer Inst. 2000;92(1):61.
Dr. Dunaief is a speaker, author and local lifestyle medicine physician focusing on the integration of medicine, nutrition, fitness and stress management. For further information, visit www.medicalcompassmd.com or consult your personal physician.





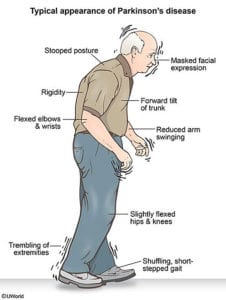 When we typically think of using CoQ10, a coenzyme found in over-the-counter supplements, it is to compensate for depletion from statin drugs or due to heart failure. Doses range from 100 to 300 mg. However, there is evidence that CoQ10 may be beneficial in Parkinson’s at much higher doses.
When we typically think of using CoQ10, a coenzyme found in over-the-counter supplements, it is to compensate for depletion from statin drugs or due to heart failure. Doses range from 100 to 300 mg. However, there is evidence that CoQ10 may be beneficial in Parkinson’s at much higher doses.









