Advocates say new budget has wins for people in recovery
By Maureen Rossi
With the opioid epidemic still endemic throughout Suffolk County and beyond, New York State senators are hoping the new state budget will mean more help for those in the throes of addiction.
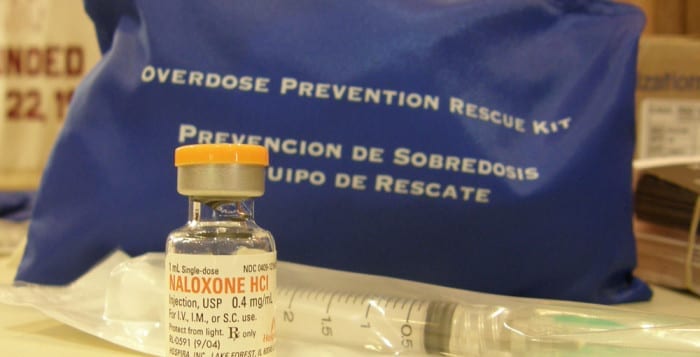
Measures woven into and passed in the state budget include increasing access for those suffering with substance use disorder to access 28-day inpatient and outpatient programs without prior insurance authorization. They also include money for a recovery high school start -up and no prior authorization for medication- assisted treatment.
“These are critical reform measures,” said New York State Sen. Monica Martinez (D-Brentwood). In addition, she touted another reform, which will require emergency rooms to enact screening, brief intervention and referral to treatment for all overdose patients before they are released. For the first time, emergency room doctors will also initiate medically-assisted treatment to overdose patients prior to their release, utilizing drugs like buprenorphine that alleviate the craving for opioids including heroin.
Martinez was joined by her Democratic colleagues at a press conference in Islandia April 12. Senators Anna Kaplan (D-Great Neck), James Gaughran (D-Northport), Kevin Thomas (D-Levittown) and Todd Kaminsky (D-Long Beach) gathered at THRIVE Long Island, a community center for people in addiction recovery whose funding was a legislative win three years back.
The Island’s Democrats were joined by stakeholders to celebrate critical initiatives passed in this year’s state budget to combat Long Island’s pernicious opioid epidemic. Those stakeholders include parents of those lost to the epidemic, those in recovery and those in the prevention and addiction field, including the CEO of Family & Children’s Association Jeffrey Reynolds, of Smithtown.
“There is still much work to be done to combat the opioid epidemic we are seeing here on Long Island,” Martinez added. She looked to Reynolds to the right of the podium and shared that he was tenacious in getting the Long Island’s senators’ attention as the hours dwindled in budget meetings. “He used social media and tagged every single one of us and let us know what funding was missing in the budget.”
Kaplan said the crisis affects every community, every school and every community.
“Too many innocent souls have been lost to this disease, they have been failed time and again,” Kaplan said. “We are done with half-measures — we will do everything we can to help people get into long-term recovery.”
One such measure included and passed in the budget was the funding of another THRIVE center for Nassau in Hempstead. The doors are scheduled to open next month.
Kaminsky met with some Long Island parents who lost loved ones to the epidemic prior to the budget process. Figures released by the addiction experts on Long Island put that figure at 3,400 since 2010.
“When a parent tells you the story of how they found their child (dead), you want to make sure another parent doesn’t experience that,” said Kaminsky.
When it came to budget negotiations that lasted around the clock, the state senator said they would not take no for an answer.
Suffolk County has long been a powerhouse when it comes to shining a light on the opioid epidemic and taking legislative measures to address it. Packages of historic bills have been pushed through statewide by Suffolk County advocates. The county is one of the state’s hardest hit counties and they were the first county in the country to file a lawsuit against Purdue Pharma, the makers of the drug OxyContin.
Reynolds addressed the senators on behalf of the sixty-plus advocates present. “ ‘Thank you’ seems insufficient. You promised on campaign trails you would do good for Long Island. Thank you so much for your efforts,” he stated.
However, Reynolds promised that he and the Long Island advocacy movement will always ask the senators to do more.