I am educator, an advocate and most importantly a parent who lost her only child to the disease of addiction. Unfortunately, I know I am not alone. The truth is: I stand with more than 72,000 other parents who grieve the loss of their child to an overdose.
When I speak publicly about addiction issues and look out at people, I see a small piece of me. When I look at your child, I see the beautiful potential of what could have been my child. If only mental health and the disease of addiction had the same basic human right to health care as other illnesses. I hope that by sharing my son’s story, I can create a future where all people are treated equally, no matter their ability or disability.
My son Vincent was sensitive, kind, funny and insightful. He was popular, played almost every sport, and his teachers always said he brought conversations to the next level and stood up for those who couldn’t stand up for themselves. I will always stand tall and be proud of the person my son was.
The one thing that most people never knew was that, no matter how hard he tried, Vincent still battled with serious mental health issues: ADHD, trichotillomania (hair-pulling disorder), anxiety and low self-esteem, which eventually led to a deep depression. Even though Vincent had a family that absolutely adored him and everyone he met thought he was handsome, smart and funny, Vincent … never saw himself that way. Children need to be taught how to communicate and be given a variety of strategies to cope in today’s world. We have to work together. It needs to be at the family, school and community level.
Vincent started smoking marijuana in high school. Toward the end of my son’s life, he shared that “pot” had been his gateway drug to stronger drugs. After high school, he was hanging around with a different crowd. During college, his “A” grades started to falter. Then, he lost his job. Something wasn’t right. I searched his room and found what I feared most: Oxycodone had become Vincent’s drug of choice. We had heated discussions that oxycodone was extremely dangerous and addictive. He would show me research that denied it. As we all know, powerful companies can find ways around the law and can state just about anything they want and get away with it.
The oxycodone amplified my son’s anxiety and depression. He began to isolate himself. He could hardly get himself to go to work or even out of the house. Vincent tried to self-detox and get drug free on his own, failing several times.
Finally, Vincent agreed his addiction was out of his control. I had so much hope he was going to get the treatment he desperately needed. Over the course of just one year, prior to my son passing away, he would get denied by the insurance company over four times!
The insurance company stated he didn’t fit “medical necessity.” First, he had supportive parents. Second, he was motivated to get better. By the third denial, I filed a complaint with the attorney general’s office. They were able to get my son 14 days. 14 days … is such a short time to physically and emotionally overcome addiction, and certainly not enough time for Vincent. My son came out and soon relapsed. This time to heroin.
After battling with the insurance company for months, they finally approved my son. Regrettably, unbeknownst to us, insurance companies are allowed to back-deny services within 30 days of approval. After detox and 14 days, my son was back-denied, stating he had no other mental health illnesses, was highly motivated to get better, and had a supportive family. He was crying that he needed more time. He was extremely anxious and severely depressed. They placed Vincent on anti-anxiety and anti-depression medication, even though my son was denied treatment due to not having any mental health illnesses.
My son was trying to get better. He went to out-patient almost every day, met weekly with his counselor, and attended meetings at night.
In the next few weeks, Vincent stayed drug free … he was beginning to be himself again. However, without getting the services he desperately needed and deserved, my son relapsed and bought drugs unknowingly laced with the deadly drug fentanyl. My son Vincent had no chance. I lost my shiny star, my beautiful son, Vincent on Sept. 13, 2017. Last month would have been his 28th birthday.
Vincent’s battle is one like too many others. In his honor, I advocate for change. He had so many barriers making it so difficult to get the help he needed: whether it be getting denied Suboxone for detox, incorrect information to determine appropriate services, or getting the Vivitrol shot to help prevent relapse. No one should ever have to fight so hard for the basic human right to health care.
Insurance companies need to be held accountable. They need to cross reference information for accuracy prior to denying inpatient treatment. They need to comply with the Mental Health Parity and Addiction Equity Act. Federal law states that anyone with a mental health illness or the disease of addiction should get the same basic human rights to healthcare as those who have regular medical conditions.
I couldn’t imagine if my son or anyone’s child had a regular health disease such as diabetes, a heart condition or cancer that they would get denied the medical care they needed, if they had a supportive family and were motivated to get better.
Over 200 loved ones die from an overdose every single day. We don’t have the luxury of time. In order to create any meaningful change, we need you to be a part of making a difference in our community. Your voice needs to be heard. It is so powerful and very important. If you truly want to see change … Reach out to your local and state representatives, ask them what their action plan is, and hold them accountable. Let them know how important it is for you and your children to have a future where everyone has the same right to get the care they need to be healthy.
It is my hope that by sharing my son’s story, I can raise awareness, encourage the importance of communication, education and most importantly equality for basic human right to healthcare.
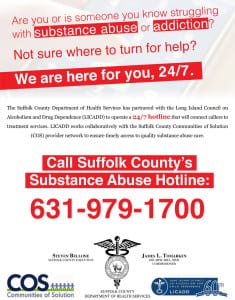
Sharon Richmond lives in Northport and is part of the Town of Huntington’s Opioid Task Force. She is also a member of the Northport-East Northport Drug and Alcohol Task Force. She works closely with F.I.S.T (Families In Support of Treatment), LICADD (Long Island Council on Alcoholism and Drug Dependence), FCA (Family and Children’s Association), the North Shore CASA (Coalition Against Substance Abuse) and Nassau County Heroin Prevention Task Force. She is a teacher at North Shore Schools in Nassau County.