Medical Compass: Is it a heart attack?
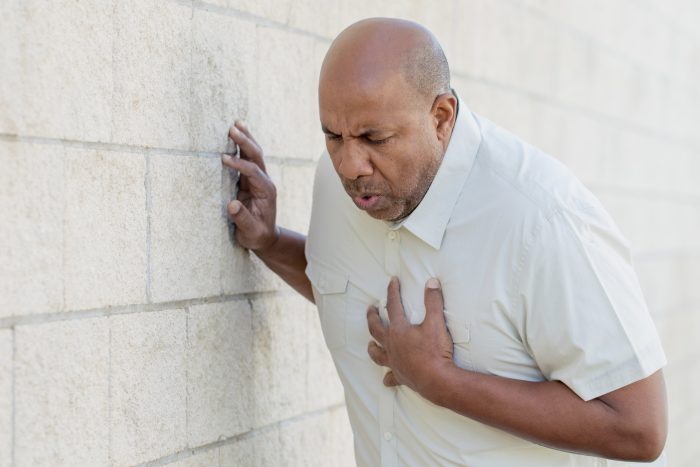
Chest pain is only one of many possible symptoms.
By David Dunaief, M.D.

Each year, 805,000 people in the U.S. have heart attacks, or myocardial infarctions —about one every 40 seconds (1). These statistics traverse race and gender lines, even though symptoms may be experienced differently. Outcomes for those having a heart attack are significantly better if they receive immediate medical attention. First, however, you need to recognize the symptoms.
What are symptoms of a heart attack?
The most recognizable symptom is chest pain. However, there are a number of other, more subtle, symptoms such as discomfort or pain in the jaw, neck, back, arms and epigastric, or upper abdominal areas. Others include nausea, shortness of breath, sweating, light-headedness and tachycardia (racing heart rate).
Unfortunately, less than one-third of people know these symptoms (2). About 10 percent of patients present with atypical symptoms — without chest pain — according to one study (3).
It is not only difficult for the patient but also for the medical community, especially the emergency room, to determine who is having a heart attack. Fortunately, approximately 80 to 85 percent of chest pain sufferers are not having a heart attack. More likely, they have indigestion, reflux or other non-life-threatening ailments. However, don’t hesitate to seek immediate medical attention; it’s better to have a medical professional rule out a heart attack than to ignore one.
Are heart attack symptoms different for men and women?
There has been much discussion about whether men and women have different symptoms when it comes to heart attacks. Several studies speak to this topic.
There is data showing that, although men have heart attacks more commonly, women are more likely to die from a heart attack (4). In a Swedish study, after having a heart attack, a significantly greater number of women died in the hospital or near-term when compared to men. The women received reperfusion therapy, artery opening treatment that consisted of medications or invasive procedures, less often than the men.
However, recurrent heart attacks occurred at the same rate, regardless of sex. Both men and women had similar findings on an electrocardiogram. This was a study involving approximately 54,000 heart attack patients, with one-third being women.
One theory about why women receive less aggressive treatment when first presenting in the ER is that they have different and more subtle symptoms — even chest pain symptoms may be different. But, is this true? Not according to several studies.
In one observational study of 2,500 patients with chest pain, results showed that, though there were some subtle differences, when men and women presented with this main symptom, it was of a similar nature (5). There were 34 chest pain characteristic questions used to determine if a difference existed. These included location, quality or type of pain and duration. Of these, there was some small amount of divergence: the duration was shorter for a man (2 to 30 minutes), and pain subsided more for men than for women. The authors concluded that determination of heart attacks with chest pain symptoms should not factor in the sex of patients.
This trial involved an older population; patients were a median age of 70 for women and 59 for men, with more men having had a prior heart attack. The population difference was a conspicuous weakness of an otherwise solid study, since age and previous heart attack history are important factors.
In the GENESIS-PRAXY study, another observational study, the median age of both men and women was 49. Results showed that chest pain remained the most prevalent presenting symptom in both men and women (6). However, of the patients who presented without distinct chest pain and with less specific EKG findings, significantly more were women than men.
Those who did not have chest pain symptoms may have experienced back discomfort, weakness, discomfort or pain in the throat, neck, right arm and/or shoulder, flushing, nausea, vomiting and headache. If the patients did not have chest pain, regardless of sex, the symptoms were diffuse and nonspecific.
Some studies imply that as much as 35 percent of patients do not present with chest pain as their primary complaint (7).
What should you do if someone is having a heart attack?
Call 911 immediately, and have the patient chew an adult aspirin (325 mg) or four baby aspirins, provided they do not have a condition that precludes taking aspirin. The purpose of aspirin is to thin the blood quickly, but not if the person might have a ruptured blood vessel. The 911 operator or emergency medical technician who responds can help you determine whether aspirin is appropriate.
What are the most frequently occurring heart attack symptoms to watch for?
Most patients have chest pain, and both men and women have similar types of chest pain. However, this is where the simplicity stops and the complexity begins. The percentage of patients who present without chest pain seems to vary significantly depending on which study you review — ranging from less than 10 percent to 35 percent.
Non-chest pain heart attacks have a bevy of diffuse symptoms, including obscure pain, nausea, shortness of breath and light-headedness. This is seen in both men and women, although it occurs more often in women. It’s important to recognize heart attack symptoms, since quick action can save your life or that of a loved one.
References:
(1) Circulation. 2022;145(8):e153–e639. (2) MMWR. 2008;57:175–179. (3) Chest. 2004;126:461-469. (4) Int J Cardiol. 2013;168:1041-1047. (5) JAMA Intern Med. 2014 Feb. 1;174:241-249. (6) JAMA Intern Med. 2013;173:1863-1871. (7) JAMA. 2012;307:813-822.
Dr. David Dunaief is a speaker, author and local lifestyle medicine physician focusing on the integration of medicine, nutrition, fitness and stress management. For further information, visit www.medicalcompassmd.com or consult your personal physician.