By Daniel Dunaief
Many research efforts search for clues about the signals or processes that turn healthy cells into something far worse. Scientists look at everything from different genes that are active to signs of inflammation to the presence of proteins that aren’t typically found in a system or organ.
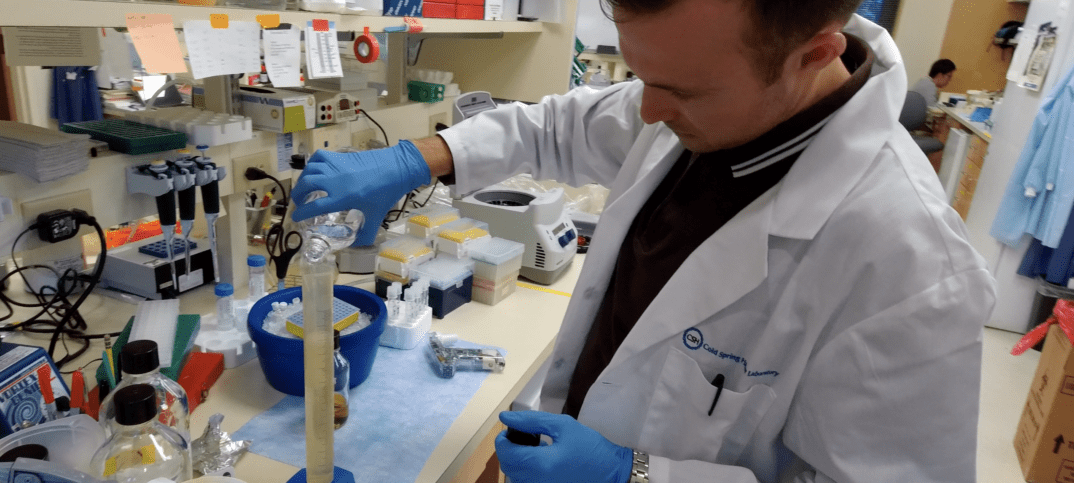
Tim Somerville, a postdoctoral researcher in Chris Vakoc’s laboratory at Cold Spring Harbor Laboratory, recently took a close look at a specific protein whose presence in a high concentration in pancreatic cancer typically worsens the expectations for a disease with an already grim prognosis.
This protein, called P63, has a normal, healthy function in skin cells for embryos and in maintaining normal skin for adults, but it doesn’t perform any important tasks in the pancreas.
Somerville wanted to know whether the protein appeared as a side effect of the developing cancer, like the appearance of skinny jeans someone wears after a diet starts working, or whether it might be a contributing cause of the cancer’s growth and development.
“What was unclear was whether [the higher amount of P63] was a correlation, which emerges as the disease progresses, or something more causal,” he said, adding that he wanted to find out whether “P63 was driving the more aggressive features” of pancreatic cancer.
Somerville increased and decreased the concentration of P63 in tissue cells and organoids, which are copies of human tumors, hoping to see whether the change had any effect on the cancer cells.
The postdoctoral researcher knocked out the amount of P63 through the use of CRISPR, a gene-editing technique. He also overexpressed P63, which is also a transcription factor.
“From those complementary experiments, we were able to show that P63 is driving a lot of the aggressive features of cancer cells,” Somerville concluded. “Rather than being a correlation that’s observed, it is functionally driving the cancer itself.”
Somerville recently published his research in the journal Cell Reports.
As a transcription factor, P63 recognizes specific DNA sequences and binds to them. With P63, Somerville observed that it can bind to DNA and switch on many genes that are active in the worse form of pancreatic cancer. He and his collaborators describe P63 as a master regulator of the gene program.
Pancreatic cancer is often discovered after the irreversible conversion of normal, functional cells into a cancerous tumor that can spread to other organs. It also resists chemotherapy. Research teams in the labs of Vakoc and Dave Tuveson, the director of the Cancer Center at CSHL, and other principal investigators at CSHL and elsewhere are seeking to understand it better so they can develop more effective treatments.

Vakoc was impressed with the work his postdoctoral researcher performed in his lab. Somerville is “one of the most scholarly young scientists I have ever met,” Vakoc explained in an email. “He is simply brilliant and thinks deeply about his project and is also driven to find cures for this deadly disease.”
At this point, Somerville is pursuing why P63 is activated in the pancreas. If he can figure out what triggers it in the first place, he might be able to interfere with that process in a targeted way. He also might be able to think about ways to slow it down or stop the disease.
The form of P63 that is active in the pancreas is not a mutated version of the protein that functions in the skin. If scientists tried to reduce P63, they would need to develop ways to suppress the cancer promoting functions of P63 without suppressing its normal function in the skin.
Many of the genes and proteins P63 activates are secreted factors and some of them contribute to inflammation. Indeed, researchers are exploring numerous ways inflammation might be exacerbating the progression of cancer.
P63 is also active in other types of cancer, including lung, head and neck cancers. Frequently, elevated levels of P63 in these other forms of cancer also lead to a worse prognosis.
Somerville explained that the changes P63 makes in a pancreatic cancer cell may expose new weaknesses. By studying cells in which he has overexpressed the protein, he hopes to see what other addictions the cells may have, which could include a reliance on other proteins that he could make compounds to target.
A resident of Huntington, Somerville has worked in Vakoc’s lab for three years. While he has spent considerable time studying P63, he is also looking at other transcription factors that are involved in pancreatic cancer.
Somerville wants to contribute to the discovery of why one form of pancreatic cancer is so much worse than the other. “If we can understand it, we can find new ways to stop it,” he said.
Originally from Manchester, England, Somerville is working in the United States on a five-year visa and plans to continue contributing to Vakoc’s lab for the next couple of years. At that point, he will consider his options, including a potential return to the United Kingdom.

Somerville appreciates the opportunity to work on pancreatic cancer with Vakoc and with Tuveson, whose lab is next door. The researcher is enjoying his time on Long Island, where he takes walks, enjoys local restaurants and, until recently, had been playing on a Long Island soccer team, which played its matches in Glen Cove.
For Somerville, Cold Spring Harbor Laboratory has exceeded his high expectations. “The research that goes on here and the interactions you can have at meetings” have all contributed to a “great experience,” he said.
Somerville is excited to be a part of the pancreatic cancer team.
“With the work from [Tuveson’s] lab and ours, we’re finding new things we didn’t know,” he said. “It’s only when you understand those different things and the complexity that you can start thinking about how to tackle this in a more successful way. If the research carries on, we’ll make improvements in this disease.”