NSAIDs and acetaminophens are not risk-free
By David Dunaief, M.D.

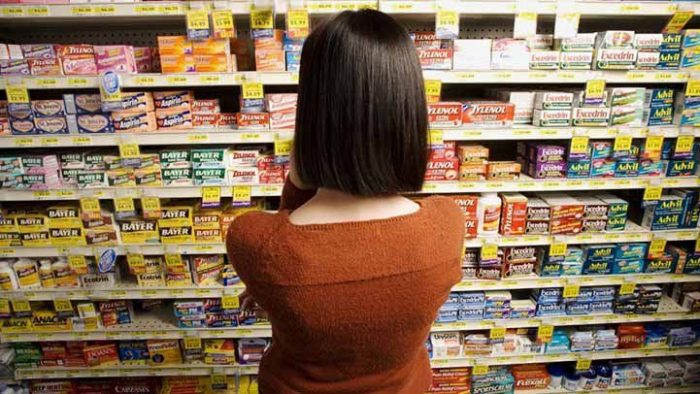
What’s in your medicine cabinet? If you’re like most people, you have your typical “go-tos” for pain relief, fever or inflammation. You might have aspirin or other NSAIDs (non-steroidal anti-inflammatory drugs) and acetaminophen (Tylenol).
Familiar NSAIDs include ibuprofen (Advil, Motrin) and naproxen sodium (Aleve). Over 70 million prescriptions for NSAIDs are written each year in the U.S., and Americans consume more than 30 billion doses, once over-the-counter (OTC) use is factored in (1).
According to a poll of these regular users of OTC NSAIDs, a substantial number — 60 percent — were unaware of their dangerous side effects (2). Acetaminophen is used frequently, as well. On a weekly basis, one quarter of Americans take it. Unfortunately, many think of these drugs as relatively benign. In fact, I find that until I specifically ask about their use, most patients don’t include them in a list of their medications.
NSAID risks
Unfortunately, NSAIDs, according to the Centers for Disease Control and Prevention, are responsible for 7,600 deaths annually and 10 times that number in hospitalizations (3). These are not medications that should be taken lightly.
NSAIDs increase the risk of several maladies, including heart attacks, gastrointestinal bleeds, exacerbation of diverticular disease, chronic arrhythmias (abnormal heartbeats) and erectile dysfunction. In some instances, the cardiovascular effects can be fatal.
These risks prompted the FDA to strengthen the warning labels on non-aspirin NSAID labels, advising that those taking NSAIDs should immediately seek medical attention if they experience chest pain, shortness of breath or trouble breathing, weakness in one part or side of their body, or slurred speech (4).
Adverse side effects of NSAIDs
In a case control study using the UK Primary Care Database, chronic users of NSAIDs between ages 40 and 89 had a significantly increased risk of a serious arrhythmia (abnormal heartbeat) called atrial fibrillation (5).
Interestingly, chronic users were defined as patients who took NSAIDs for more than 30 days. Those patients who used NSAIDs more than 30 days had a 57 percent increased risk of atrial fibrillation. A Danish study reinforces these results after the first month of use (6). This is not very long to have such a substantial risk. For patients who used NSAIDs longer than one year, the risk increased to 80 percent.
Caution should be used when prescribing NSAIDs or when taking them OTC. Atrial fibrillation is not an easy disease to treat.
NSAIDs also increase the risk of mortality in chronic users. Older patients who have heart disease or hypertension (high blood pressure) and are chronic NSAIDs users are at increased risk of death, according to an observational study (7). Compared to those who never or infrequently used them over about 2.5 years, chronic users had a greater than twofold increase in death due to cardiovascular causes. High blood pressure was not a factor, since the chronic users actually had lower blood pressure. Yet I have seen with my patients that NSAID use can increase blood pressure.
Is acetaminophen better?
Acetaminophen does not cause gastrointestinal bleeds, arrhythmias and deaths due to cardiovascular events that NSAIDs can. However, the Food & Drug Administration announced in 2011 that acetaminophen should not exceed 325 mg every four to six hours when used as a prescription combination pain reliever (4). The goal is to reduce and avoid severe injury to the liver, which can cause liver failure.
There is an intriguing paradox with acetaminophen: Hospitals typically dispense regular-strength 325-mg doses of the drug, whereas OTC doses frequently are found in extra-strength 500-mg tablets, and often the suggested dose is two tablets, or 1 gram. At the FDA’s request, Tylenol lowered its recommended daily dosage for extra strength Tylenol to no more than 3 grams a day to lower the risk of liver damage.
I have patients who have exceeded this, thinking that, because it is OTC, this is “safe.” Unfortunately, this is not true and can be dangerous.
The FDA’s recommendations for limiting the dose result from a conglomeration of data. For instance, one study that showed acute liver failure was due primarily to unintentional overdoses of acetaminophen (8). Accidental overdosing is more likely to occur when taking acetaminophen at the same time as a combination sinus, cough or cold remedy that also contains acetaminophen. OTC and prescription cold medications can contain acetaminophen.
Of course, if you already suffer from liver damage or disease, you should consult with your physician before taking any medications.
In order to be aware of potentially adverse events, you have to be your own best advocate and read labels. Remember to tell your physician if you are taking OTC medications.
If you are a chronic user of NSAIDs or acetaminophen because of underlying inflammation, you may find an anti-inflammatory diet, which is usually plant-based, is an effective alternative.
References:
(1) Medscape.com, 2021 Oct 21 (emedicine.medscape.com/article/816117-overview). (2) J Rheumatol. 2005;32;2218-2224. (3) Annals of Internal Medicine, 1997;127:429-438. (4) fda.gov (5) Arch Intern Med. 2010;170(16):1450-1455. (6) BMJ 2011;343:d3450. (7) Am J Med. 2011 Jul;124(7):614-620. (8) Am J Gastroenterol. 2007;102:2459-2463.
Dr. David Dunaief is a speaker, author and local lifestyle medicine physician focusing on the integration of medicine, nutrition, fitness and stress management. For further information, visit www.medicalcompassmd.com.