Increasing potassium may improve health outcomes
By David Dunaief, M.D.

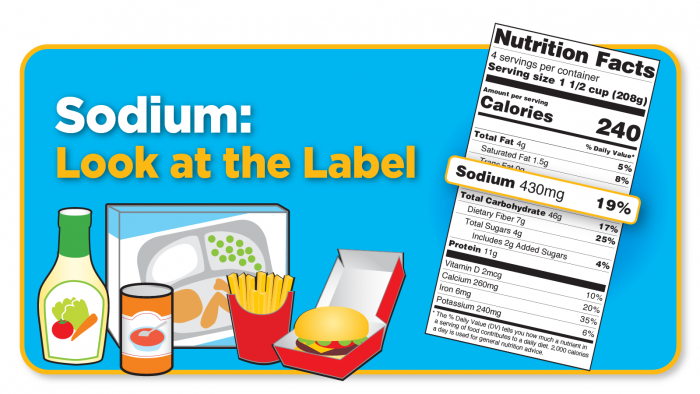
Most Americans consume far too much sodium — an average of 3400 mg per day, which is well over the 2300 mg per day recommended upper limit for teens and adults (1). It’s become such an issue that the FDA is working with food manufacturers and restaurants to drive these numbers down (2).
If you don’t have hypertension, what difference does it make? Sodium can have a dramatic effect on your health, regardless of your blood pressure.
It’s hard to avoid, with sodium hiding even in foods that don’t taste salty, like bread products and salad dressings. Other foods with substantial amounts of sodium include cold cuts and cured meats, cheeses, poultry, soups, pasta, sauces and, of course, snack foods. Packaged foods and restaurant meals are where most of our consumption occurs.
In contrast, only about two percent of people consume enough potassium in their diets (3). According to the National Institutes of Health, target potassium intake is between 2600 mg and 3400 mg for adult women and men, respectively.
How are sodium and potassium related?
A high sodium-to-potassium ratio increases your cardiovascular disease risk by 46 percent, according to a 15-year study of more than 12,000 participants (4).
A more recent analysis of over 10,000 participants followed for almost nine years tested sodium and potassium excretion, a more reliable measure of intake, and found that higher sodium excretion, lower potassium excretion, and a higher sodium-to-potassium ratio were all associated with a higher cardiovascular risk (5). Each daily incremental increase of 1000 mg in sodium excretion was associated with an 18 percent increase in cardiovascular risk.
To improve your overall health, you might need to shift your sodium-to-potassium balance so that you consume more potassium and less sodium. And if you struggle with — or are at risk for — high blood pressure, this approach could help.
Why lower your sodium consumption?
Two studies illuminate the benefits of reducing sodium in high and normal blood pressure patients, ultimately preventing cardiovascular disease, including heart disease and stroke.
The first was a meta-analysis that evaluated data from 34 randomized clinical trials, totaling more than 3,200 participants. It demonstrated that salt reduction from 9-to-12 grams per day to 5-to-6 grams per day had a dramatic effect. Blood pressure in both normotensive and hypertensive participants was reduced by a significant mean of −4.18 mm Hg systolic (top number) and −2.06 mm Hg diastolic (bottom number) (6).
When looking solely at hypertensive patients, the reduction was even greater, with a systolic blood pressure reduction of −5.39 mm Hg and a diastolic reduction of −2.82 mm Hg.
The researchers believe that the more we reduce salt intake, the greater the blood pressure reduction. The authors recommend further reduction to 3 grams per day as a long-term target and hypothesize that the effects on blood pressure will most likely result in a decrease in cardiovascular disease.
In the second study, a meta-analysis of 42 clinical trials including both adults and children, there was a similarly significant reduction in both systolic and diastolic blood pressures (7). Both demographics experienced a blood pressure reduction, although the effect was greater in adults. Interestingly, an increase in sodium caused a 24 percent increased risk of stroke incidence but, more importantly, a 63 percent increased risk of stroke mortality. The risk of mortality from heart disease increased by 32 percent alongside an increase in sodium.
Isn’t too little sodium a risk?
Some experts warn that sodium levels that are too low can be a problem. While this is true, it’s very rare, unless you have a health condition or take medication that depletes sodium. Since sodium is hiding everywhere, even if you don’t add salt to your food, you’re probably consuming more than the recommended amount of sodium.
Why focus on potassium consumption?
In a meta-analysis involving 32 studies, results showed that as the amount of potassium was increased, systolic blood pressure decreased significantly (8). When high blood pressure patients consumed foods containing 3.5 to 4.7 grams of potassium, they experienced an impressive −7.16 mm Hg reduction in systolic blood pressure. Anything more than this amount of potassium did not provide additional benefit. Increased potassium intake also reduced stroke risk by 24 percent.
Blood pressure reduction was greater with increased potassium consumption than with sodium restriction, although this was not a head-to-head comparison. The good news is that it’s easy to increase your potassium intake; it’s found in many whole foods and is richest in fruits, vegetables, beans and legumes.
So, what’s the bottom line? Decrease your sodium intake and increase your potassium intake from foods to strike a better sodium-to-potassium balance. As you reduce your sodium intake, give yourself a brief period to adapt; it takes about six weeks to retrain your taste buds.
References:
(1) Dietary Reference Intakes for Sodium and Potassium. Washington (DC): National Academies Press (US); 2019 Mar. (2) fda.gov. (3) nih.gov. (4) Arch Intern Med. 2011;171(13):1183-1191. (5) N Engl J Med 2022;386:252-263. (6) BMJ. 2013 Apr 3;346:f1325. (7) BMJ. 2013 Apr 3;346:f1326. (8) BMJ. 2013; 346:f1378.
Dr. David Dunaief is a speaker, author and local lifestyle medicine physician focusing on the integration of medicine, nutrition, fitness and stress management. For further information, visit www.medicalcompassmd.com or consult your personal physician.









 By now, most of us have been hit over the head with the fact that too much salt in our diets is unhealthy. Still, we respond with “I don’t use salt,” “I use very little,” or “I don’t have high blood pressure, so I don’t have to worry.” Unfortunately, these are myths. All of us should be concerned about salt or, more specifically, our sodium intake.
By now, most of us have been hit over the head with the fact that too much salt in our diets is unhealthy. Still, we respond with “I don’t use salt,” “I use very little,” or “I don’t have high blood pressure, so I don’t have to worry.” Unfortunately, these are myths. All of us should be concerned about salt or, more specifically, our sodium intake.




